Redesigned ACO REACH Model Strives to Provide Better, Whole-Person Care
CMS announced a redesigned ACO model that better reflects the agency’s vision of achieving equitable health outcomes.
THE VBP Blog

The Centers for Medicare & Medicaid Services (CMS) announced a redesign of the Global and Professional Direct Contracting Model (GPDC). The ACO Realizing Equity, Access, and Community Health (ACO REACH) Model will be put in place.
According to CMS, the ACO REACH model supposedly better reflects the agency’s goal of creating a health system that achieves equitable outcomes through high-quality, whole-person care. This is essential for both Medicaid-only and dual-eligible beneficiaries as it can promote health equity and access to quality care in communities that need it most. Throughout this blog, we will take a deeper dive into the new ACO model and analyze how it differs from its predecessor and what that could mean for improved care.
CMS Transitioning to ACO REACH Model
Beginning January 1, 2023, the Global and Professional Direct Contracting Model (GPDC) Model is being renamed and revamped under the ACO REACH model. It will run for four performance years (PY), through PY 2026.
The goal of this model is to improve the quality of care for Medicare beneficiaries through care coordination. Connecting health care providers and beneficiaries is a priority of the Administration and the new model will hopefully support that.
“CMS is testing a redesigned model because accountable care organizations make it possible for people in Traditional Medicare to receive greater support managing their chronic diseases, facilitate smoother transitions from the hospital to their homes, and ensure beneficiaries receive preventive care that keeps them healthy,” said Liz Fowler, PhD, JD, CMS Deputy Administrator and Director of the CMS Innovation Center. “Under the ACO REACH Model, health care providers can receive more predictable revenue and use those dollars more flexibly to meet their patients’ needs — and to be more resilient in the face of health challenges like the current public health pandemic. The bottom line is that ACOs can improve health care quality and make people healthier, which can also lead to lower total costs of care.”
The change comes as the GPDC Model faced some criticism from members of Congress. Some concerned stakeholders alleged that the GPDC Model could lead to the privatization of Medicare. As investor-owned entities were reportedly taking ownership of Direct Contracting Enterprises (DCEs), access to quality healthcare was being threatened.
In response to concerns from stakeholders, CMS Administrator Chiquita Brooks-LaSure reiterated the organization’s focus, “The Biden-Harris Administration remains committed to promoting value-based care that improves the health care experience of people with Medicare, Medicaid, and Marketplace coverage. To fulfill that commitment, CMS, through the Innovation Center, is testing new models of health care service delivery and payment to improve the quality of care that people receive, including those in underserved communities.”
CMS followed up, stating, “Models that do not meet these core principles will be redesigned or will not move forward.”
ACO REACH vs. GPDC Model – What Changed?
So, what really changed and how does the ACO REACH model address concerns about the GPDC Model?
As the chart below shows, the new ACO REACH, touts an advanced focus on health equity, with increased governance, vetting, monitoring, and transparency.
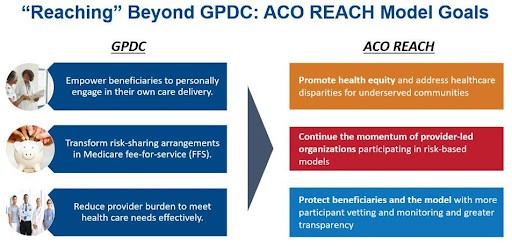
Source: The Centers for Medicare & Medicaid Services
In addition to the goals of the ACO REACH model, there are additional changes from the GPDC model. While the GPDC Model has no policies promoting health equity. The new model requires all REACH ACOs to create a Health Equity Plan. This plan must include the identification of health disparities and the actions intended to mitigate the disparities identified. ACOs must also establish a health equity benchmark and collect demographic and social needs data of beneficiaries. This is encouraging as it will help hold participating ACOs accountable for addressing health equity and proving care for unmet social needs.
The other main change from the GPDC Model is enhanced transparency and governance. Under the old model, participating providers only needed to hold 25% of the governing board voting rights, whereas, under the ACO REACH Model, they must hold 75% of the governing board voting rights. The new model also requires the beneficiary representative and consumer advocate to be separate people and hold voting rights. Under the GPDC Model, these individuals could be the same person and were not required to hold voting rights.
There are also more thorough monitoring and compliance requirements for ACOs under the REACH model. The increased monitoring will include:
- Annual assessment to determine if beneficiaries are being shifted into or out of Medicare Advantage
- Analysis of risk scores to identify potential inappropriate coding
- Monitoring potential anti-competitive actions
- Utilizing data analytics to compare changes in beneficiaries’ access to care
- Annual audits of REACH ACO contracts with providers to learn more about downstream arrangements so concerns can be addressed
- Investigate provider and beneficiary complaints and grievances
While these governance and monitoring changes might seem insignificant, they directly address the concerns that stakeholders had over the GPDC Model’s risk of the privatization of Medicare.
Under ACO REACH, the benchmark is also increasing for ACOs serving a higher proportion of underserved beneficiaries. This will help ensure that all Medicare beneficiaries are served, thus reducing health disparities. Withholds for quality are also reduced under the new model, which encourages more provider participation compared to the prior model. This is particularly important as we look to the dual eligible individuals. Medicare beneficiaries dually enrolled in Medicaid are five times more likely to have a disability and 2.6 times more likely to be of a minority race or ethnicity. They also often have worse health outcomes and less access to quality medical care. The standard risk adjustment and payment model used to pay ACOs and Medicare Advantage plans often underpredicts costs of dual enrollees, which undermines care of this population, but ACO REACH risk adjust benchmarks are based on dual eligibility status, which should help close the health equity gap.
Typically, one of the challenges VBP faces is providing capital upfront so organizations can build and redesign care delivery systems. With the ACO REACH “health equity benchmark” providing an additional $30 per beneficiary per month for serving more underserved beneficiaries, CMS strives to close this gap to reduce health disparities for the high needs’ population, including the dually eligible. This is especially important as ACOs are becoming more common for dual eligible individuals and it is essential that these individuals get access to equitable and quality care.
While there are stark differences between ACO REACH and the GPDC Model, those currently participating in the GPDC Model are not being completely cut out of the redesign. However, ACOs must agree to comply with all the ACO REACH Model requirements by the start of PY2023 to continue participating. Those interested will need to sign new participation agreements but will not be required to re-apply to participate in the ACO REACH model.
Advocates Perspective
The new ACO REACH launching in 2023 appears to have the requirements and processes in place to promote health equity and facilitate access to quality care for Medicare beneficiaries through VBP payments. It is also essential to consider the importance of health equity and access to quality care for the vulnerable Medicaid-only and dual eligible individuals. Could this new ACO REACH model provide a successful blueprint for the future of integrated care? While only time will tell through the four-year trial period, it is encouraging to see CMS actively listening to stakeholders, beneficiaries, and participants as they continue the shift to value-based payments from traditional fee-for-service Medicare. As the healthcare industry transitions to VBP, stakeholder engagement and quality of care must be at the forefront and we are glad to see CMS acting accordingly. While some say ACO REACH does not go far enough, with increased governance and additional monitoring and transparency, we are excited to follow the progress of the model and continue to assess how it performs.
Onward!
Share This Blog!
Get even more insights on Linkedin & Twitter

About the Author
Fady Sahhar brings over 30 years of senior management experience working with major multinational companies including Sara Lee, Mobil Oil, Tenneco Packaging, Pactiv, Progressive Insurance, Transitions Optical, PPG Industries and Essilor (France).
His corporate responsibilities included new product development, strategic planning, marketing management, and global sales. He has developed a number of global communications networks, launched products in over 45 countries, and managed a number of branded patented products.

About the Co-Author
Mandy Sahhar provides experience in digital marketing, event management, and business development. Her background has allowed her to get in on the ground floor of marketing efforts including website design, content marketing, and trade show planning. Through her modern approach, she focuses on bringing businesses into the new digital age of marketing through unique approaches and focused content creation. With a passion for communications, she can bring a fresh perspective to an ever-changing industry. Mandy has an MBA with a marketing concentration from Canisius College.