Provider and Payer Partnerships Making a Positive Impact on Health Outcomes
Health payers are collaborating with providers to improve health outcomes
THE VBP Blog

In order to achieve some of the best health outcomes possible, partnerships are being formed. And we’re not just talking about limited partnerships where organizations or providers are receiving referrals. Partnerships between healthcare providers and payers, healthcare payers and for-profit companies, and partnerships involving organizations that offer important non-medical services are all important. In this blog, we will look at some of the recent partnerships that have sprung up in the healthcare world and how these partnerships are helping to improve health outcomes.
Healthcare Payers Partnerships Making a Big Impact
Collaboration of care is key when it comes to driving better outcomes for patients. That is why the first partnership we will look at is the one between Partners Health Management (PHM) and North Carolina Medicaid Managed Care.
Partners Health Management is a local management entity (LME), a provider led entity that manages Medicaid, state and local funds for mental health, intellectual/developmental disabilities, and other aspects of healthcare. The North Carolina Department of Health and Human Services (NCDHHS) partners with PHM to manage behavioral health care services.
As more and more networks and providers are utilizing 360-degree views of members to offer more personalized care, PHM takes matters a bit further. While others only address physical healthcare, PHM also incorporates directories of social services to ensure providers can offer whole-person care.
“We’re focused on providing positive outcomes for patients. Partners (PHM) helps providers give care to members,” stated Michael Kincaid, Chief Information Officer of PHM. “Providers submit their claims and get authorizations from us before they provide services and get reimbursed. With us, they receive authorization and then can submit a claim and check the status of that claim. If they can’t provide a specific service that is beyond their capabilities, then they can find another provider to help their patient. It’s all about providing the best possible care: We want to make this process as easy and efficient as possible.”
This allows the provider flexibility in the services they deliver and acknowledges the importance of identifying and supporting needs that may not have been in the original person-centered plans. It is through these partnerships and collaboration that consumers are truly able to get the care—both medical and non-medical—that they need for a positive health outcome.
North Carolina Medicaid Partnering with Non-Medical Providers
North Caroline Medicaid is an example of healthcare payers partnering with providers. North Carolina DHHS is partnering with social service providers to address social determinants of health to improve health outcomes.
Through the Healthy Opportunities Pilots program, North Carolina DHHS is putting Medicaid dollars towards non-medical evidence-based interventions that impact overall health. CMS authorized $650 million in funds over five years for four domains: housing, food, transportation, and interpersonal violence/toxic stress.
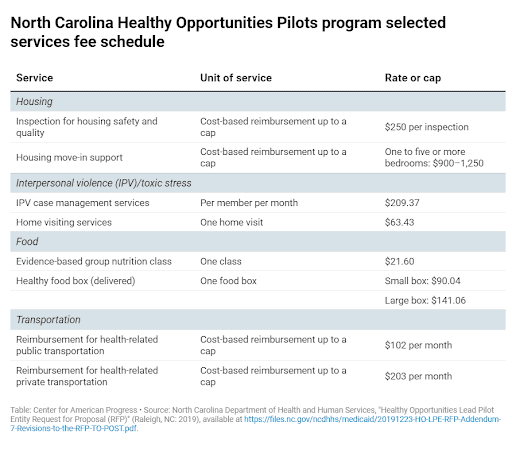
The chart above shows how providers get paid. But how does a human service organization get involved in the program? Network leads are established that have deep community roots to facilitate collaboration and build partnerships between healthcare payers and providers. One network lead will operate in each pilot region, and human service organizations that address these non-medical needs can contract with the region’s network lead. This program launched in March 2022 and we will be keeping an eye on its progress.
Healthcare Providers and For-Profits Creating Beneficial Partnerships for Consumers
Partnerships between healthcare providers and for-profit companies are also important in the healthcare arena. Recently, there are several of note.
Blessing Health System based in Quincy, Illinois, recently partnered with Biofourmis to create a hospital-at-home program. Biofourmis is a health technology company that uses advanced software and data to enhance virtual care offerings. Together, Blessing Health System and Biofourmis will work together to deliver acute-level hospital care at-home. Not only does this allow hospital beds to remain open for more critically ill patients, but hospital-at-home programs also lead to lower readmissions rates, reduced costs, and better patient satisfaction.
This is unique in that it is part of the Rural Home Hospital program. The program tests whether the home-hospital model can be adapted for rural settings. One in five Americans live in rural areas, but these are often underserved by the federal government and are closing in record numbers. Through this partnership, care is being expanded to rural areas to improve access to quality health care.
Another example of this is the 2020 partnership between Aetna and Papa. Papa is a for-profit company that provides non-medical companionship services. The partnership started in Florida, where 80% of eligible Florida Medicare Advantage members reported feeling severely lonely and depressed. Through the partnership, Papa provides companionship benefits to address social isolation issues. This falls into the social determinants of health realm, and relationships like this are key to addressing SDoH and improving overall health outcomes.
After using the Papa companionship benefit that Aetna provides members, 86% of participating members in Florida reported an improvement in their feelings of loneliness. Based on the positive results, Aetna and Papa expanded the partnership to an additional seven states – Nevada, California, Illinois, Michigan, North Carolina, Pennsylvania, and Indiana. Results through the expansion we equally positive. 62% of Aetna PPO members and 52% of Aetna Dual Eligible Special Needs Plan (D-SNP) members that utilized the services in 2021 reported feeling less lonely and happier overall. With mental health having a big impact on overall health, this is significant and shows how health plans can meet member needs through contracting with private companies.
Advocates Perspective
It is encouraging to see the impact that these partnerships are having on health outcomes. Through collaboration and partnerships between healthcare payers and healthcare providers, consumers are able to get the medical and non-medical care that they need to achieve a positive health outcome. At XtraGlobex, we advocate for consumers and favor collaborations of provider led organizations, like the LMEs in North Carolina. We are also encouraged to see behavioral health and healthy equity addressed in these partnerships.
Onward!
Share This Blog!
Get even more insights on Linkedin & Twitter

About the Author
Fady Sahhar brings over 30 years of senior management experience working with major multinational companies including Sara Lee, Mobil Oil, Tenneco Packaging, Pactiv, Progressive Insurance, Transitions Optical, PPG Industries and Essilor (France).
His corporate responsibilities included new product development, strategic planning, marketing management, and global sales. He has developed a number of global communications networks, launched products in over 45 countries, and managed a number of branded patented products.

About the Co-Author
Mandy Sahhar provides experience in digital marketing, event management, and business development. Her background has allowed her to get in on the ground floor of marketing efforts including website design, content marketing, and trade show planning. Through her modern approach, she focuses on bringing businesses into the new digital age of marketing through unique approaches and focused content creation. With a passion for communications, she can bring a fresh perspective to an ever-changing industry. Mandy has an MBA with a marketing concentration from Canisius College.