OhioRISE Program Launched This Month to Provide Specialized Managed Care to Youth with Complex Needs
The program aims to keep families together by providing access to HCBS for children with the most complex behavioral health challenges
THE VBP Blog

July 21, 2022 –
Managing care and support services for children with complex behavioral needs can be extremely difficult. Unfortunately, getting comprehensive care to assist can also be hard to obtain and very costly. Recently, Ohio has taken steps to rectify this and keep families together by launching the OhioRISE (Resilience through Integrated Systems and Excellence) program.
OhioRISE is a specialized managed care program for youth with complex behavioral health and multisystem needs. The plan is designed to ensure appropriate assessments to identify needs, individualized care plans including in-home and community services, and coordination of services across community providers, systems, and agencies.
In this blog, we will take a look at the recently launched OhioRISE managed care plan and how it is being used to provide whole-person care to children with complex behavioral health challenges.
Complex Behavioral Health Situations Are Difficult for Families to Manage
In some instances, obtaining behavioral and mental health care for children with complex needs is so difficult or expensive that parents will relinquish custody to the state. They do this to ensure that their children will get the required, unaffordable behavioral and mental health care that the child requires. Sometimes, in-patient treatment can cost tens, if not hundreds of thousands of dollars and parents do not have the means to cover the necessary care.
“Eight years ago, my family was in crisis. My wife and I were forced to surrender custody of our son Andrew to access necessary treatment for his extreme behavioral health needs caused by Autism and several mental illnesses. My story is not unique. Ohio Parents of multisystem youth have faced similar agonizing choices for decades,” said Mark Butler, a parent and advocate for OhioRISE.
This is not an uncommon issue. The University of Maryland Institute for Innovation and Implementation released a study entitled, Relinquishing Custody for Mental Health Services. The study found that the lack of availability and accessibility of intensive HCBS and lack of payment mechanisms for high-cost services were common factors that led to custody relinquishment.
Additionally, there is qualitative and quantitative data showing an ‘intersection’ of youth who need a greater array of services and care coordination than the current Medicaid plan provides.
Ohio took drastic action to address the issue of costly and complex care systems by devising OhioRISE. The ultimate goal of OhioRISE is to keep youth in their homes and communities by assessing for and delivering the appropriate services needed with the goal of reducing unnecessary out-of-home placement.
OhioRISE Addresses Complex Behavioral Health Needs to Keep Families Together
OhioRISE is aimed at shifting the system of care to keep more kids and families together. This is done through enhanced care coordination and access to in-home and community-based services for children with complex behavioral health needs.
“OhioRISE offers hope for thousands of Ohio families who have long struggled to find help for their children; it enables us to coordinate the care and services for at-risk kids, to better meet their emotional, behavioral, and physical needs,” said Governor DeWine in a press release announcing the launch of OhioRISE on July 1, 2022.
This child and family-centric care delivery system is available to families covered by Medicaid. Through the program, families can take advantage of intensive treatments and coordinated care, and will have everything paid for through Medicaid.
Through a partnership with Aetna Better Health of Ohio, the program will address longstanding haps in care and coordination that often leave families navigating complex systems on their own. Now, families can work through a new statewide network of care management entities that work as community-based experts in navigating and coordinating care.
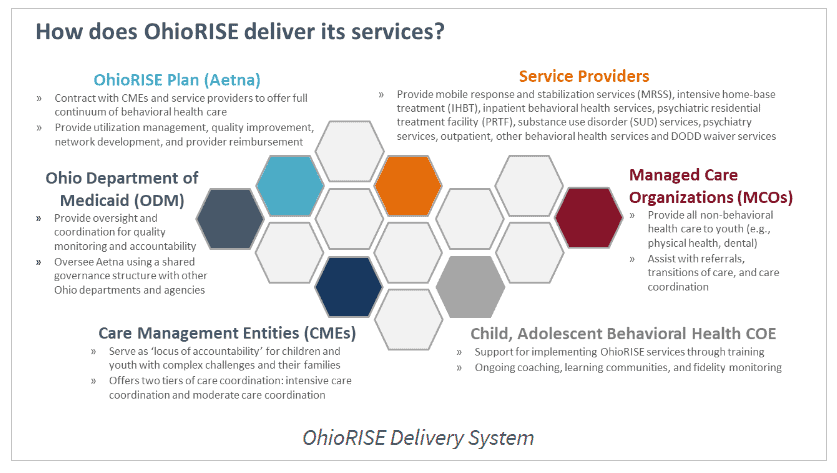
Members will be provided a coordinator through Aetna or a care management entity (CME) for assistance in obtaining the resources they need to work with multiple community systems such as juvenile justice, child protection, developmental disabilities, schools, mental health, and addiction, and more.
Eligibility for OhioRISE
OhioRISE eligibility is for individuals that are eligible for Ohio Medicaid, are under 20 years of age, and require significant behavioral health treatment needs. This is measured using the Ohio Children’s Initiative Child and Adolescent Needs and Strengths (CANS) tool was chosen as the system-wide assessment tool.
“Using the CANS right from the outset of the OhioRISE implementation, will help ensure that the program’s effectiveness and impact is being measured right from the get-go,” says Dan Warner, Ph.D., the executive director of Community Data Roundtable, an organization that promotes a data-driven human services system. “This data will help advocates, providers, government and managed care make sure the needs of families are being adequately addressed as the system unfolds.”
For ease of integration, the Ohio Children’s Initiative CANS Information Technology (IT) System was launched for child-service systems throughout Ohio. This system establishes eligibility into the OhioRISE program by submitting a CANs assessment, document assessments and updates, and supports the goal of “one child, one CANS” to ensure that children do not go through multiple assessments. With this IT system, providers and systems will hopefully be able to collaborate effectively to provide whole-person care.
CANS will not only be used to assess eligibility, but it will also guide treatment plan development and inform intensity of care determinations.
Services and Supports Provided Through OhioRISE
The plan covers all medically necessary Medicaid-covered behavioral healthcare services for children and youth. Eligible children and youth will still receive all the mental health and substance use disorder services currently covered by Ohio Medicaid, but there is an extensive list of new and improved services offered through OhioRISE.
Services will be provided on an individualized basis that is informed by the child’s or youth’s and family’s voice and choice, under the guidance of the care coordinator. The additional services available through OhioRISE include:
- Moderate and Intensive Care Coordination
- Mobile Response and Stabilization Service (MRSS)
- Intensive Home-Based Treatment (IHBT)
- Psychiatric Residential Treatment Facility (PRTF)
- Behavioral Health Respite
- Primary Flex Funds
- In-state Psychiatric Residential Treatment Facilities (PRTFs) – launching in 2023
What’s unique about OhioRISE is that the newly added and expanded services and supports shirt the focus from lower intensity and out-of-home care to intensive community and home-based services. Instead of placing children in institutional settings, they are able to remain in the comfort of their homes to receive necessary care. Studies have shown that those receiving care outside of institutional settings and from home actually see better outcomes.
As of July 1, 2022, approximately 5,500 youth and children in Ohio were proactively enrolled in OhioRISE. By the end of year 1, the state expects at least 50,000 children to be enrolled, with the potential of reaching 60,000.
Advocates Perspective
OhioRISE is a step in the right direction for care coordination and delivery. Through this program, at least 50,000 youth and children in Ohio will be able to receive complex and necessary services and supports that will allow them to remain at home with their families. What’s unique about this program is the enhanced coordination of care that will assist families in navigating complex and often siloed medical and community systems. The coordination ensures that whole-person care is received through collaboration between providers and systems, which can improve overall outcomes. Through CMEs and care coordinators, youth and children in Ohio can receive the services and supports that they require through Medicaid to remain comfortably at home and in their communities.
Onward!
Share This Blog!
Get even more insights on Linkedin & Twitter

About the Author
Fady Sahhar brings over 30 years of senior management experience working with major multinational companies including Sara Lee, Mobil Oil, Tenneco Packaging, Pactiv, Progressive Insurance, Transitions Optical, PPG Industries and Essilor (France).
His corporate responsibilities included new product development, strategic planning, marketing management, and global sales. He has developed a number of global communications networks, launched products in over 45 countries, and managed a number of branded patented products.

About the Co-Author
Mandy Sahhar provides experience in digital marketing, event management, and business development. Her background has allowed her to get in on the ground floor of marketing efforts including website design, content marketing, and trade show planning. Through her modern approach, she focuses on bringing businesses into the new digital age of marketing through unique approaches and focused content creation. With a passion for communications, she can bring a fresh perspective to an ever-changing industry. Mandy has an MBA with a marketing concentration from Canisius College.