Providers in Home Health VBP Model Outperformed Counterparts in 2020
Providers participating HHVBP model performed 7% better in 2020 than non-participating providers in 9 states
THE VBP Blog

The Centers for Medicare & Medicaid Services (CMS) Center for Medicare & Medicaid Innovation (CMMI) recently released the 5th Annual Report for the Evaluation of the Home Health Value-Based Purchasing (HHVBP) Model. Conducted by Arbor Research Collaborative for Health for CMS, the report analyzes how provider organizations participating in the HHVBP model fared versus non-participating provider organizations.
As you’ll recall from our Healthcare at Home VBP Blog Series, the HHVBP model was launched in 9 states back in 2016. Arizona, Florida, Iowa, Massachusetts, Maryland, Nebraska, North Carolina, Tennessee, and Washington were all randomly selected for the model with 3% to 11% of home health provider organizations participating. The model was designed to examine whether a VBP plan would improve the delivery of home health care services. After years of data collection and analysis, CMS and CMMI deemed the program to be a success and proposed a nationwide expansion of the model. In the final CY 2022 HH PPS rule, CMS announced that the HHVBP model would be expanded nationwide in 2023.
The nationwide expansion of the Home Health VBP model is a step in the right direction and bodes well for other groups, including LTSS. In this blog, we will look at how the HHVBP model fared in year 5 specifically and what these successes could mean for other types of VBP plans.
HHVBP Model Still Showing Promising Results in 2020
The 5th Annual Report covered results and lessons learned from the 2020 reporting year. According to the results, those participating in the HHVBP model performed 7% better than non-participating providers when looking at Total Performance Scores (TPS).
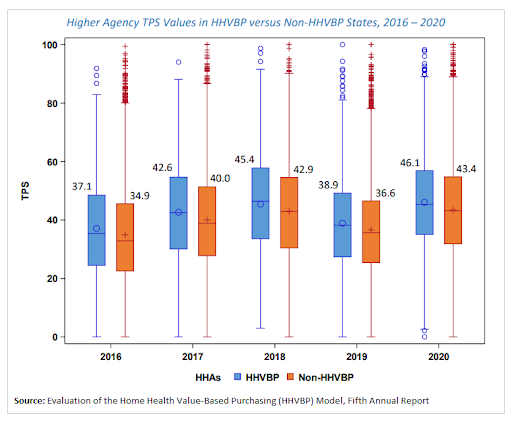
A TPS is a comprehensive score that examines quality of care and determines reimbursement rates for providers. Payment adjustments are determined based on how the agency performs against others in the state across 12 measures that make up the TPS. TPS scores for participating home health providers have continually increased every year since 2016, which means that the model’s payment adjustment increased every year.
In addition to overall TPS scores increasing, total spending decreased. Home health provider organizations participating in the model saved Medicare just shy of $950 million from 2016 to 2020. The decrease in spending is attributed to a reduction in unplanned hospitalizations and admissions to skilled nursing facilities.
Both improved quality of care and lowered costs lend credibility to the model, but there were other benefits as well. Medicare beneficiaries who received care from a provider participating in the HHVBP model saw more improvement in functional status than those who did not. In addition, overall health outcomes over time improved for those utilizing providers participating in the HHVBP model. These positive results are what led CMS to permanently expand the HHVBP model nationwide starting January 1, 2023.
HHVBP Success Resonates with LTSS VBP Plans
The promising results of the HHVBP model and nationwide expansion in 2023 highlight how value-based payment models can transform care by improving overall outcomes and reducing spending, all while individuals receive care from the comfort of their homes. While the VBP model has yielded great results for the home health sector, can long-term services and supports (LTSS) also benefit?
Many state Medicaid programs are aiming to improve the cost-effectiveness and quality of LTSS by changing how providers are paid for those services. State Medicaid agencies are shifting from fee-for-service (FFS) payment systems to value-based payment models. This is significant because over 13 million Americans use LTSS to assist with daily living activities that they are unable to perform themselves as a result of aging, disability, or chronic illness.
Many of these individuals seek to receive care where they live, instead of in an institutional setting so they can remain comfortable and engaged in the community. However, despite the fact that the majority of individuals receiving LTSS use home-and community-based services (HCBS) providers, many of the current state Medicaid LTSS VBP models involve providing care in nursing facilities. That is beginning to change as states are rebalancing spending from institutional care to home- and community-based services to improve the beneficiary experience and manage costs more effectively.
This shift came about when the Medicaid Innovation Accelerator Program (IAP) was launched and began to look into Value-Based Payment for HCBS. The IAP was created to accelerate ongoing innovation in Medicaid and increase the number of states moving towards delivery system reform. Through the VBP for HCBS track, states worked towards planning, designing, and developing a VBP strategy. The Medicaid IAP provided program support that included aligning financial incentives, identifying quality measure strategies, engaging with stakeholders, and designing VBP for HCBS strategies.
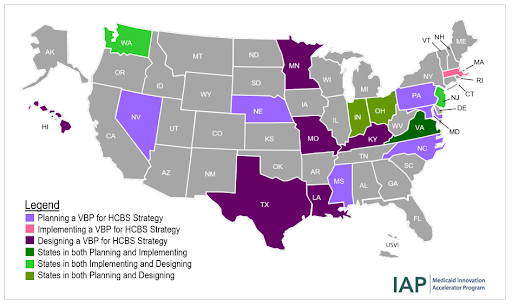
As the map above shows, at the end of the various programs, participants were in various stages of design, planning, and implementation and there is still a lot of work to be done. The HHVBP model results thus far highlight the potential that utilizing HCBS providers for LTSS recipients can have on health outcomes, and how those services can be incorporated into a successful VBP model that incentivizes quality care, while also cutting costs.
Advocates Perspective
As LTSS and HCBS value-based payment plans expand, it is important for states and health plans to continue working to improve the quality and coordination of care. The HHVBP model success and subsequent nationwide expansion in 2023 shows that value-based payments can work in settings beyond standard medical facilities and it is important to examine how this can be replicated for other sectors. As the majority of individuals want to age peacefully at home and receive care where they are most comfortable, there must be incentives for providers to offer this type of care. This is especially important as hospital at home and other home care initiatives have resulted in an improvement in health outcomes. As additional LTSS and HCBS VBP plans roll out and expand, we will keep an eye on them and continue to advocate for stakeholder involvement and thoughtful consideration of health equity.
Onward!
Share This Blog!
Get even more insights on Linkedin & Twitter

About the Author
Fady Sahhar brings over 30 years of senior management experience working with major multinational companies including Sara Lee, Mobil Oil, Tenneco Packaging, Pactiv, Progressive Insurance, Transitions Optical, PPG Industries and Essilor (France).
His corporate responsibilities included new product development, strategic planning, marketing management, and global sales. He has developed a number of global communications networks, launched products in over 45 countries, and managed a number of branded patented products.

About the Co-Author
Mandy Sahhar provides experience in digital marketing, event management, and business development. Her background has allowed her to get in on the ground floor of marketing efforts including website design, content marketing, and trade show planning. Through her modern approach, she focuses on bringing businesses into the new digital age of marketing through unique approaches and focused content creation. With a passion for communications, she can bring a fresh perspective to an ever-changing industry. Mandy has an MBA with a marketing concentration from Canisius College.