Value-Based Payments Growth Trends...Are You Ready?
THE VBP Blog

We are exploring value-based growth trends this week. Current data shows Medicaid managed care programs using value-based payments programs have experienced steady growth over the past few years, 67% of Medicaid’s 74 million consumers are enrolled in some type of health plan and 55% of Medicaid budgets are going to health plan payments.
Of all Medicaid MCO respondents, 93% utilized a value-based purchasing (VBP) or alternative payment model (APM), according to a survey done in 2020 by Medicaid Innovation. That is an increase of 14% since 2017. The survey covered 2019 data taken from Medicaid managed care organizations (MCOs), and the trend continues
Enrollment Growth Trends
Enrollment also continues to climb, leading to a higher population receiving value-based reimbursed services and care. In 2010, 49% of the Medicaid managed care population was enrolled and that number increased to 73% in 2019. The states with their population enrolled grew from 25 to 37 in that same time period. Some states offer comprehensive managed care delivery systems and require eligible individuals to sign up where other states exclude certain people based on where they live or if they have a disability and others even have an opt-out program.
Payment Structures
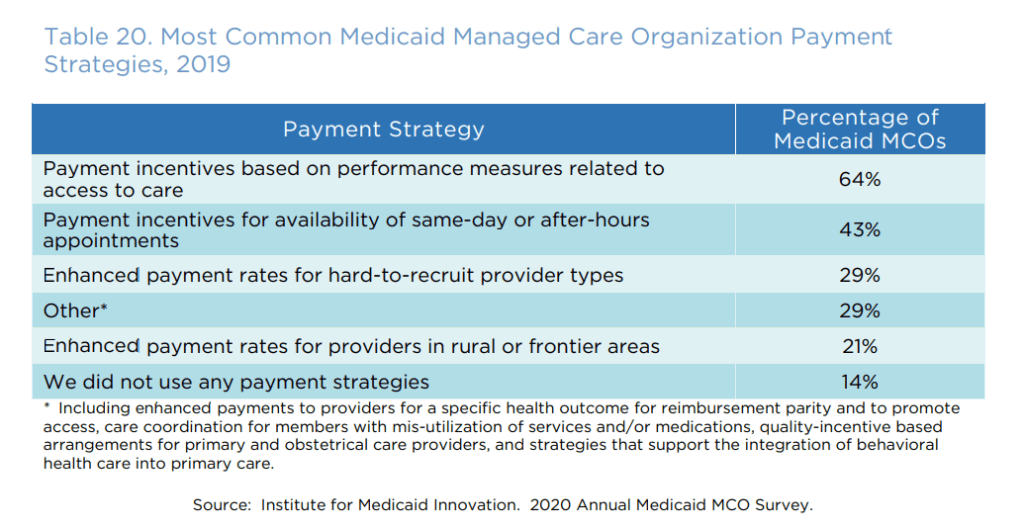
Payment structures are continuing to change with the Medicaid health plans, with all MCOs covering 250,000 consumers or more using VBPs and APMs. In 2018, 33% of Medicaid payments were linked to a value-based structure. 17% of those were APMs built off a fee-for-service (FFS) structure and 10% were pay-for-performance. [Resource: State Strategies to Promote Value-Based Payment through Medicaid Managed Care – Bailit Health]
In September 2020, CMS announced new initiatives to expand value-based care options to the Medicaid beneficiaries. This guidance includes an assessment of key lessons learned from early adoption including multi-payer participation, delivery system readiness, stakeholder engagement, and the scope of financial risk to providers. CMS lays out options for states to choose from to allow for flexibility as they implement their own program. This lays out a guidance as Medicaid and value-based programs move forward with their individual growth trends. The ambitious plan intends for 50% of Medicaid payments and 100% of Medicare payments to be value-based by 2025.
Advocate's Perspective
While most of what we reported in this blog relates to physical health, we continue to see this trend picking up steam and becoming irreversible. We want to continue to make sure consumers’ needs and well-being are paramount in the development of these new reimbursement structures. Our concerns rise to an even higher level when we consider provider readiness. As advocates, we want to see states and health plans collaborate with providers to prepare for successful transitions and growth into these new payment models. For the providers, we continue to urge you to look at your state’s guidelines and how you can better prepare yourself and your organization for the future. Identify the current Medicaid plans, learn about which value-based mandates are in place, create a review of your programs and services and how they can shift to an alternative payment model or value-based structure, and finally build a strategy of how you will pivot to stay successful for the future.
Share This Blog!
Get even more insights on Linkedin & Twitter

About the Author
Fady Sahhar brings over 30 years of senior management experience working with major multinational companies including Sara Lee, Mobil Oil, Tenneco Packaging, Pactiv, Progressive Insurance, Transitions Optical, PPG Industries and Essilor (France).
His corporate responsibilities included new product development, strategic planning, marketing management, and global sales. He has developed a number of global communications networks, launched products in over 45 countries, and managed a number of branded patented products.

About the Co-Author
Mandy Sahhar provides experience in digital marketing, event management, and business development. Her background has allowed her to get in on the ground floor of marketing efforts including website design, content marketing, and trade show planning. Through her modern approach, she focuses on bringing businesses into the new digital age of marketing through unique approaches and focused content creation. With a passion for communications, she can bring a fresh perspective to an ever-changing industry. Mandy has an MBA with a marketing concentration from Canisius College.