Health Equity is Shifting to the Forefront
Health inequities result from race, ethnicity, disability, sexual orientation, socioeconomic status, geography, and other factors.
THE VBP Blog

In a perfect world, all individuals would be able to achieve their full health potential. For so many people in the United States and around the world, that is not the case. This is because health inequities exist throughout to health care system and all individuals are not provided access to the quality care that they need and deserve.
The United States ranks 43rd in the world on the health indicator of average life expectancy at birth and this becomes even worse when you break that down further demographically. Between certain racial and ethnic populations, there can be up to a seven-year difference in life expectancy in the United States.
How can we become a healthier nation? By achieving health equity for all individuals. In this blog, the first of a two-part series on health equity, we will take a deeper dive into health equity, to understand what it is, how it impacts health outcomes and its recent shift to the forefront of the industry.
What is Health Equity?
Health equity is defined by the Centers for Medicare & Medicaid Services (CMS) as “the attainment of the highest level of health for all people, where everyone has a fair and just opportunity to attain their optimal health regardless of race, ethnicity, disability, sexual orientation, gender identity, socioeconomic status, geography, preferred language, or other factors that affect access to care and health outcomes.”
More simply put, health equity is achieved when every person has the opportunity to attain their full health potential and no one is disadvantaged due to socially determined circumstances. This goes beyond simply having access to a doctor. Health inequity is rooted in everything from race and disability to socioeconomic status and sexual orientation.
Why Does Health Equity Matter?
Health disparities have a huge impact on health outcomes. That being said, it is important to note that not all health differences are disparities. A health difference becomes a health disparity when it is the result of unfair or unjust exposure to detrimental health and social factors.
For example, the health difference between the aging population and the younger population is not considered a health disparity. But, differences in health between white mothers and black mothers, who are less likely to receive quality prenatal care and experience higher rates of death in childbirth, are a health disparity.
Health disparities as a result of race and ethnicity go far beyond maternal health. For example, for approximately 40% of quality measures in the AHRQ’s National Healthcare Quality and Disparities Report, Blacks, American Indians, and Alaska Natives received worse care than Whites. For over 33% of quality measures in the report, Hispanics received worse care than whites.
The chart below from The Commonwealth Fund shows the vast differences in overall health scores as well.
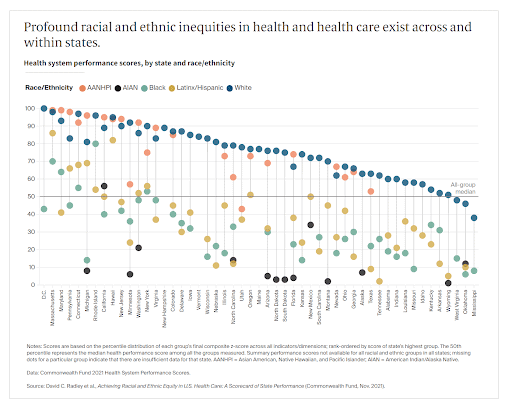
However, not all disparities are race-related. Location and income also have an impact. For nearly a quarter of quality measures, residents of large central metropolitan areas received worse care than residents of large fringe metropolitan areas. The chart above also shows that geographical differences have an impact on overall health scores, even among the same race.
As you can see, many factors can impede an individual’s ability to attain their full health potential. Unfortunately, many health disparities are deeply rooted in the healthcare system and greatly affect not only the quality of care but also health outcomes. That is why health equity is being brought to the forefront as a major focus for the healthcare industry.
Health Equity is Shifting to the Forefront
As you can see, it is essential to include health equity measures in the industry to ensure optimal health outcomes for all. But health equity is a complex challenge so how can it truly be achieved?
According to the WHO Thirteenth Global Programme of Work, “Identifying health inequalities and their drivers is essential for achieving health equity.”
This starts with data collection and analysis. Health inequities must be recorded, monitored, and studied to identify the difference in health between different subgroups. That can help provide evidence on who is being left behind when it comes to health policies and programs.
This is something that is becoming more prevalent as CMS, CMMI, and policymakers are starting to act.
“Advancing health equity is the core work of the Centers for Medicare & Medicaid Services. We can’t achieve our health system goals until everyone can attain the highest level of health,” said CMS Administrator Chiquita Brooks-LaSure in a press release.
Center for Medicare and Medicaid Innovation (CMMI) Director Liz Fowler also stated, “You can expect future innovation center models to have features like ACO REACH, like requirements for health equity plans,” during AHIP’s 2022 National Conference on Health Policy and Government Health Programs.
These are promising statements when it comes to the advancement of health equity, but actions speak louder than words. In our next blog, we will take a deeper dive into what CMS, CMMI, and policymakers are actually doing to address the issue of health inequities and disparities.
Advocates Perspective
It is encouraging to see that healthcare leaders in the United States are committed to take action to promote health equity. Decades of policy choices made by federal, state, and local leaders have led to economic suppression, unequal access to education, and segregation, which have all contributed to worse health outcomes for many people. We will be keeping a close eye on what CMS, CMMI, and policymakers are doing to right these wrongs, and help ensure that everyone in the United States has equitable access to care and the ability to achieve their full health potential.
Onward!
Share This Blog!
Get even more insights on Linkedin & Twitter

About the Author
Fady Sahhar brings over 30 years of senior management experience working with major multinational companies including Sara Lee, Mobil Oil, Tenneco Packaging, Pactiv, Progressive Insurance, Transitions Optical, PPG Industries and Essilor (France).
His corporate responsibilities included new product development, strategic planning, marketing management, and global sales. He has developed a number of global communications networks, launched products in over 45 countries, and managed a number of branded patented products.

About the Co-Author
Mandy Sahhar provides experience in digital marketing, event management, and business development. Her background has allowed her to get in on the ground floor of marketing efforts including website design, content marketing, and trade show planning. Through her modern approach, she focuses on bringing businesses into the new digital age of marketing through unique approaches and focused content creation. With a passion for communications, she can bring a fresh perspective to an ever-changing industry. Mandy has an MBA with a marketing concentration from Canisius College.