Next Generation of Ohio Medicaid Managed Care Launches
Will Ohio’s new program be success?
THE VBP Blog

March 30, 2023 – Ohio saw its first major update of Medicaid Managed Care plans since they first started in 2005. On February 1, the Next Generation Ohio Medicaid program was implemented for its 3.6 million enrollees. This new and revamped program emphasizes strong cross-agency coordination and partnership among MCOs, vendors, sister state agencies, and Ohio Department of Medicaid (ODM) to support specialization in addressing critical needs. We did touch on the roll out of this program in a 2022 blog. With this new focus on whole-person care and improved consumer experience and overall care, let’s break down the new changes.
Next Generation Procurement Process
In 2019, Ohio started the procurement process of analyzing the previous program and gathering feedback from enrollees, providers, and others to find the issues and opportunities. This also included town halls and interviews as well as written suggestions from consumers. In the end, they moved from five to seven managed care plans. Those plans were selected for their focus on social determinants of health (SDOH) and their understanding of the needs of this specific group.
Significant Changes with Next Generation Program
The state’s Next Generation program has taken the slogan, “focus on the individual and not just the business of managed care”. With that in mind, they set specific goals:
- Improve health outcomes
- Support individual wellness
- State-driven and data-informed population health strategy
- Population health strategy is a broad term for a wide range of health determinants such as access to medical care, individual behavior, and individual environments.
The foundational work needed to accomplish these goals is creating a strong coordination of care among public entities, private providers, communities, and individuals. Additionally, access to data from each of these groups is imperative to develop an effective strategy and identify opportunities for collaboration. With the overall goal being increased quality of care and ease of use for both providers and enrollees.
This chart helps break down the collaborative effort between both medical and non-medical factors that impact health.
Shifting the Healthcare Industry to VBP Is Already Yielding Positive Results
Ultimately, value-based payments can help improve patient outcomes by incentivizing healthcare providers to focus on patient outcomes and quality of care instead of just the number of services provided. By focusing on preventative care, encouraging collaboration among healthcare providers, and prioritizing patient-centered care, value-based payments are the future of the U.S. healthcare system.
In fact, value-based payment models are already making waves in the healthcare industry. For instance, the Medicare Shared Savings Program (MSSP), which incentivizes accountable care organizations (ACOs) to lower healthcare costs while meeting quality benchmarks, has shown promising results. In 2020, MSSP ACOs generated over $1.1 billion in net savings for Medicare while delivering high-quality care to millions of beneficiaries.
The Home Health Value-Based Payment (HHVBP) program has also shown promising outcomes in terms of care quality and cost efficiency. Hospital readmissions decreased by 3.6% over the first three years of the program, emergency department visits without hospitalization decreased by 4.9% during the same period, and average improvement in quality scores among participating HHAs increased by 6.2%. Improved health outcomes weren’t the only benefit. The program achieved an estimated net savings of $141 million for Medicare over its first three years, indicating improved cost efficiency. Based on these results, CMS expanded the program nationwide.
As you can see, there are many benefits to implementing value-based payment models and this just might be the key to improving the value of the U.S. healthcare system.
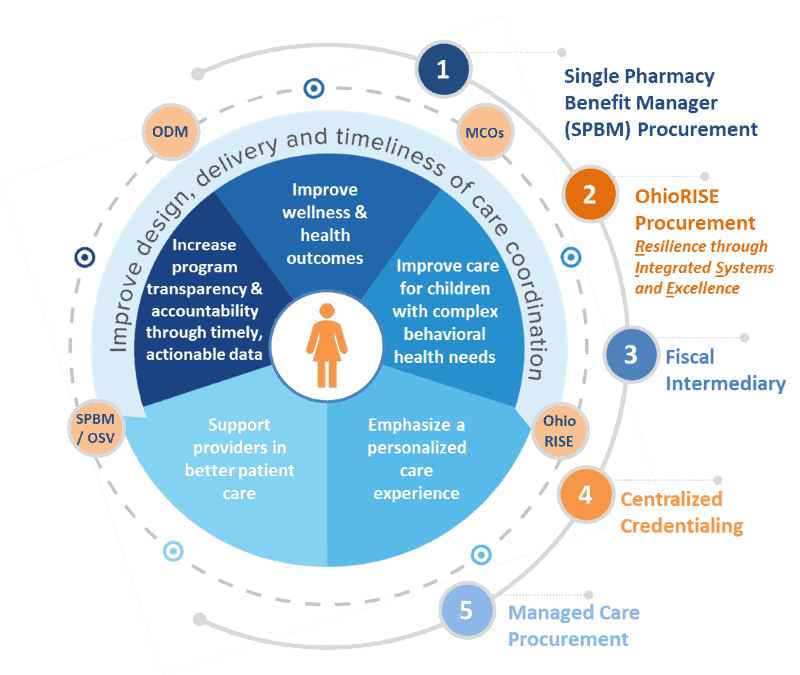
Here are some Acronym Definitions:
ODM – Ohio Department of Medicaid
MCOs – Managed Care Organizations
SPBM/ OSV – Single Pharmacy Benefits Manager / Operations Support Vendor
OhioRISE – Ohio Resilience through Integrated Systems and Excellence
To focus on the individual, the Ohio Medicaid program is using technology to create simple and easy communication directly to enrollees to create a personalized care experience. This allows each person to be treated with respect and be informed of their health care.
Modernizing Information Systems for Providers
On February 1, Ohio also launched a new Electronic Data Interchange (EDI) and Fiscal Intermediary to support providers and create a better integrated network for care. This allows providers to have one place to get credentialed and submit claims, eliminating extra paperwork and time. Managed care claims submitted via the EDI will be routed to the MCOs for processing, adjudication, and payment. Fee-for-service claims will also be processed through the EDI and paid by the FI.
High Level Care Coordination
For children and individuals with complex needs, care coordination is crucial. Next Generation promises to connect individuals with personalized and high-quality services needed for their situation.
For children with behavioral challenges, a new program called OhioRISE (Resilience Through Integrated Systems and Excellence). OhioRISE aims to shift the system of care and provide access to in-home and community-based services and high-level care coordination. We wrote an entire blog dedicated to OhioRise, you can find it here.
Next Generation Offers Increased Transparency
One of the largest challenges with any managed care program is transparency and accountability. The Next Generation program is attacking that head-on by exploring best practices and solutions. Data analytics and consumer healthcare dashboards are being developed to create real-time data and strengthen care oversight. Overall, this should provide a higher quality of care.
Advocates Perspective
After analyzing all of the different state programs throughout the year, we feel strongly that consumers will benefit from this program. Ohio took their time with a slow 3-phased roll out and focused on the large pain points such as care coordination, technology, and considering both medical and non-medical factors in how care can be given. Additionally, the Next Generation program considered what providers need to be successful and have given them time to work out kinks and figure out what changes need to happen to be successful. The supplemental program for children (OhioRISE) that has its own resources to solve unique and complex situations allows for providers to be prepared and not stretched too thin. Overall, we this has all of the foundation to be a success and provide a high level and quality of care, but time will tell.
Onward!
Share This Blog!
Get even more insights on Linkedin & Twitter

About the Author
Fady Sahhar brings over 30 years of senior management experience working with major multinational companies including Sara Lee, Mobil Oil, Tenneco Packaging, Pactiv, Progressive Insurance, Transitions Optical, PPG Industries and Essilor (France).
His corporate responsibilities included new product development, strategic planning, marketing management, and global sales. He has developed a number of global communications networks, launched products in over 45 countries, and managed a number of branded patented products.

About the Co-Author
Mandy Sahhar provides experience in digital marketing, event management, and business development. Her background has allowed her to get in on the ground floor of marketing efforts including website design, content marketing, and trade show planning. Through her modern approach, she focuses on bringing businesses into the new digital age of marketing through unique approaches and focused content creation. With a passion for communications, she can bring a fresh perspective to an ever-changing industry. Mandy has an MBA with a marketing concentration from Canisius College.