Are IDD & LTSS Sectors Getting a Boost From Value-Based Payments?
National Quality Forum (NQF) endorsed 14 NCI-IDD measures while states turn their focus to LTSS training.
THE VBP Blog

Value-based payments tie outcomes and the quality of care to compensation. This relationship incentivizes providers to provide whole-person care that creates an individualized care plan addressing both the medical and non-medical needs of individuals under their care.
Recently, VBP has been pushing into the IDD and LTSS arenas. From new quality indicators to an investment in LTSS-focused training, we are seeing positive signs that we will dive into in more detail throughout this blog.
What are Indicators?
NCI indicators are measures that assess progress or performance in various domains and sub-domains. They are designed to reflect the aims of aging, physical disabilities, and intellectual and developmental disabilities (IDD) systems.
Indicators are developed to reflect major organizational and system goals and have face validity, requirements that allow them to be used for accurate measurement purposes. These indicators provide an overall picture of how a system is performing and allow outcomes and progress to be tracked over time.
NCI Intellectual and Developmental Disabilities (NCI-IDD) consists of various domains and sub-domains that survey and measure different indicators. For example, under the Individual Outcomes Domain, falls sub-domains like Employment, Community Inclusion and Belonging, Choice and Decision Making, and Relationships, among others. Another domain looks at System Performance with Self-Direction, Service Coordination, and Access among sub-domains.
14 New IDD National Core Indicator Measures Implemented
In 2022, the National Quality Forum endorsed 14 new National Core Indicator measures. These measures came out after a rigorous review of scientific methods, panel analysis, and public comment.
Five measures are in the Person-Centered Planning (PCP) and Coordination domain. These include:
- The proportion of people who express they want a job who have a related goal in their service
plan
- The proportion of people who report their service plan includes things that are important to them
- The proportion of people who express they want to increase independence in functional skills
(ADLs) who have a related goal in their service plan
- The proportion of people who report they are supported to learn new things
- The proportion of people who report satisfaction with the level of participation in community
inclusion activities
In addition, four measures fall under the Community Inclusion domain:
- The proportion of people who reported that they do not feel lonely often
- The proportion of people who reported that they have friends who are not staff or family
members
- The proportion of people who report adequate transportation
- The proportion of people who engage in activities outside the home
Four more NCI measures are under the NQF HCBS Domain of Choice and Control. These include:
- The proportion of people who reported they chose or were aware they could request to change
their staff
- The proportion of people who reported they could change their case manager/service
coordinator
- The proportion of people who live with others who report they can stay home if they choose when others in their house/home go somewhere
- The proportion of people who report making choices (independently or with help) in life decisions
Finally, one additional NCI measure in the Human and Legal Rights domain was added:
- The proportion of people who report that their personal space is respected in the home
As you can see, these indicators go beyond traditional healthcare services, thus linking value-based care into the IDD space. These new National Core Indicators are important as they appropriately track, and thus encourage, the enhancement of quality services and supports provided to those with intellectual and developmental disabilities.
States Investing in Training to Support LTSS
LTSS is another area of healthcare that is getting a boost from VBP. New York specifically is a great example. Not only did the state launch Value-Based Payment for Managed Long Term Care Plans as a way to improve integration and coordination of care, but it also launched a plan to combat the direct care workforce crisis in home-based care.
New York-based PHI is an advocacy organization for direct care workers that is striving to secure better compensation and more comprehensive training. New York’s Medicaid Managed Long Term Care Workforce Investment Program has distributed $245 million to “retrain, recruit, and retain healthcare workers in the long-term care sector.” Results from a Health Services Research article showed that long-term care clients who received services from trained aides experienced statistically significant positive outcomes in four of seven VBP measures.
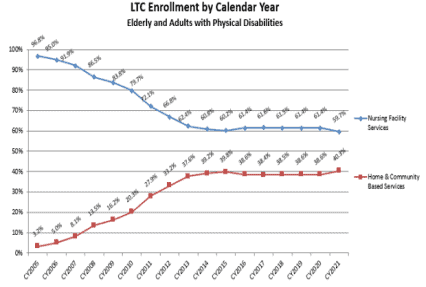
Other states like Tennessee and Maine are also addressing training in the LTSS arena. In Tennessee, through a VBP program, workers can earn stackable training credentials. These credentials help them earn competency-based badges that allow them to achieve a higher occupational designation. As the chart below shows, there has been progress in Tennessee. Seniors and adults with physical disabilities are increasingly relying on HCBS services instead of enrolling in a nursing home.
Massachusetts has also taken a unique approach by building a pipeline to direct care jobs in partnership with Northeastern University. In collaboration with the University, the state government created an employment website that connects potential job candidates with direct care jobs. Through the pilot program, a website called www.ConnectToCareJobs.com was created. That website now operates in seven states.
Pennsylvania is another great example of a state fighting for the LTSS and IDD community. To combat the direct care workforce crisis in the state, a coalition of providers and their associations to advocate with the Pennsylvania legislators to increase funding for workers supporting the most vulnerable consumers with physical and intellectual disabilities and people requiring behavioral supports. The state is facing a dire workforce crisis that is causing providers to cut programs and services. Without these services, Pennsylvanians will no longer be able to live at home, in a community home, or receive the life-sustaining services they need.
Having accurate data is also essential when examining the direct care workforce that provides LTSS services. Most nationally representative surveys of home health are almost 15 years old, according to PHI. Some states are taking the initiative to get accurate and updated data.
Texas is one example. The state has required LTSS providers to submit data on their direct care workforce since 2018. They do this through mandatory cost reports and the data provides essential information about the workforce across LTSS programs.
The state of Texas also announced a pilot program that will utilize Medicaid managed care funds to pay for LTSS for individuals with IDD, traumatic brain injuries, and similar functional needs. Through the STAR+PLUS Pilot Program (SP3), eligible individuals can receive rehabilitative therapy, home-delivered meals, socialization, personal assistance services, transportation services, and more. The National Core Indicators and Consumer Assessment of Healthcare Providers and Systems measures will be put in place to measure the performance of the program. While only time will tell how the SP3 program fares, the state has seen substantial improvement in 6 of the 20 overall indicators listed on the LTSS State Scorecard.
Through these initiatives, many driven by value-based payments and the need to continue offering quality LTSS services, individuals are able to continue receiving the services they require.
Advocates Perspective
It is encouraging to see the advancements in the IDD and LTSS spheres. These areas of healthcare have often been overlooked, but now value-based payments are tying positive outcomes and quality of care to compensation. This is causing providers to get behind the programs and invest in the services and supports that the community needs.
Onward!
Share This Blog!
Get even more insights on Linkedin & Twitter

About the Author
Fady Sahhar brings over 30 years of senior management experience working with major multinational companies including Sara Lee, Mobil Oil, Tenneco Packaging, Pactiv, Progressive Insurance, Transitions Optical, PPG Industries and Essilor (France).
His corporate responsibilities included new product development, strategic planning, marketing management, and global sales. He has developed a number of global communications networks, launched products in over 45 countries, and managed a number of branded patented products.

About the Co-Author
Mandy Sahhar provides experience in digital marketing, event management, and business development. Her background has allowed her to get in on the ground floor of marketing efforts including website design, content marketing, and trade show planning. Through her modern approach, she focuses on bringing businesses into the new digital age of marketing through unique approaches and focused content creation. With a passion for communications, she can bring a fresh perspective to an ever-changing industry. Mandy has an MBA with a marketing concentration from Canisius College.