Fresh Approach to Managed Care in NY and NC
THE VBP Blog
We’ve navigated you through 8 of the ten states with a managed care I/DD program and in this blog, we will cover the final two. We have learned a lot about the different approaches, the successful and not as successful programs, and the work that is still left to do. In our next blog, we will recap everything we have learned and what it means moving forward.
North Carolina has been working with a form of managed care since 2005, but in 2015 committed to move towards a whole-person managed care approach. Their shift towards a new program has been halted due to legislation struggles and COVID-19, but the plan looks impressive. New York also has an emerging I/DD managed care program with enrollment starting in 2018. Their Health Home/Care Coordination Organizations model is unique and their focus on high coordination efforts will be something to keep an eye on as results come in.

North Carolina
History & Current Program
Since 2005, North Carolina has managed the I/DD community through the North Carolina’s Medicaid Primary Care Case Management (PCCM) system under a fee-for-service structure. Their behavioral health and I/DD health care services are covered through a prepaid inpatient health plan (PIHP) delivered by Local Management Entities-Managed Care Organizations (LMEs/MCOs). The LME’s are responsible for “managing, coordinating, facilitating and monitoring the provision of mental health, developmental disabilities, and substance abuse services in the area they serve.”
When LME/MCOs were implemented, care coordination fell directly under them. That shift left individuals feeling like they had lost the personal touch offered by their service coordinators that they were working with before implementation. In particular, individuals with complex needs have to lean on parents or caretakers due to less contact with their service coordinator.
With this program, the goals were high-value care, improving population health, engaging providers, and creating predictable costs. High-value care is the best care possible for the patient, including optimal results for the circumstances at the right price. There was some success with creating budget predictability and addressing service gaps with a stronger provider network. With ten LME/MCOs, the main issues derived from lack of consistency and standardization, which caused administrative burdens, payment inconsistencies, and challenges navigating different systems.
Soon-to-be Managed Care Program
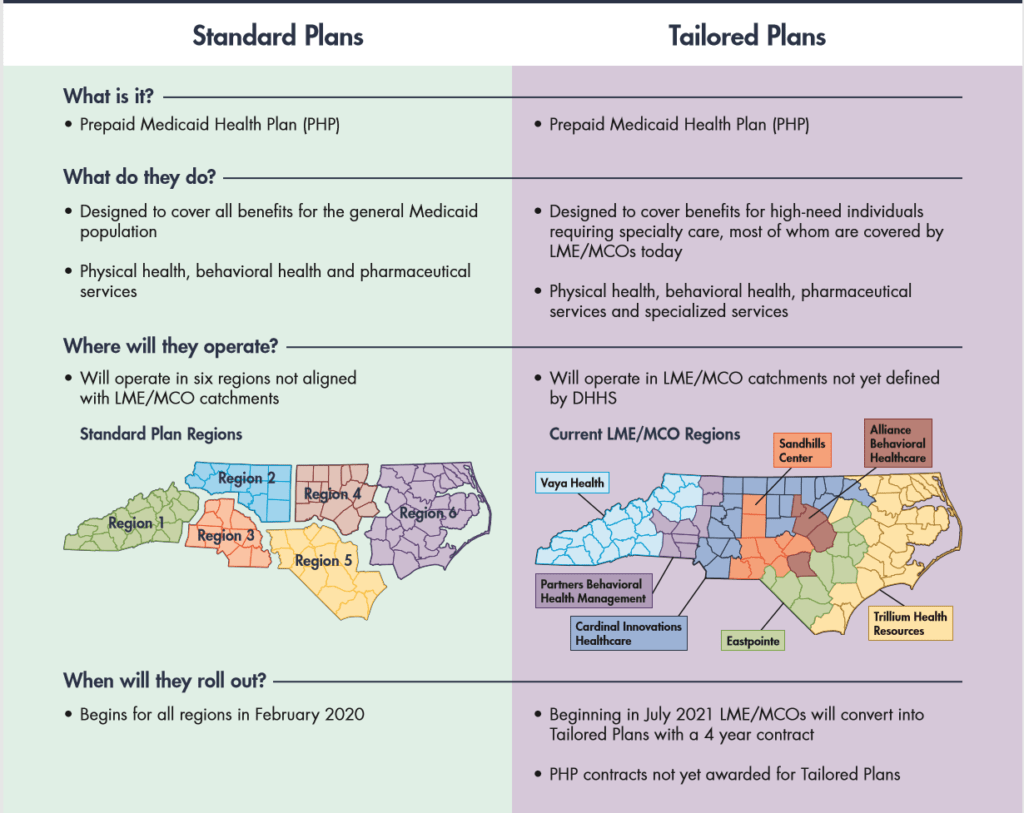
In 2015, the North Carolina General Assembly enacted legislation directing DHHS to transition Medicaid and its fee-for-service (FFS) model to managed care. In October of 2018, CMS approved NC’s 1115 Demonstration Waiver for a new Managed Care program. The program is designed to utilize two prepaid health plans (PHP)s and contracts were awarded to four entities in 2019. Phase one of the rollout will be for “standard plans” (SPs) which will be offered to the majority of beneficiaries who have less significant needs. In phase two, “tailored plans” (TPs) will focus on individuals with significant behavioral health needs, individuals with I/DD, and TBI to provide specialized services for their needs. They anticipate about 85,000 enrollees will need TPs while 1.6 million will need SPs. The original timeline anticipated all would be enrolled by 2021.
In November of 2019, the NC General Assembly did not take the necessary actions to allow the program to go live. As a result, the North Carolina Department of Health and Human Services announced a delay in the launch of their new Managed Care program that was set to launch on February 1, 2020. For now, they are still using their FFS model and benefits will stay the same. It will be difficult to restart the managed care enrollment process, so this bump could prove lethal for the program. We will keep our eyes on it.
New York
History
According to the 2018 ANCOR MLTSS white paper, since 2011, NY has been working to implement a strategy to care for the LTSS and I/DD populations. The 2011 People First Waiver proposal aimed to establish “Developmental Disability Individual Support and Care Coordination Organizations” (DISCOs). These entities were to be paid at a capitated rate and licensed as PIHPs. It also sought to create a specialized program for the I/DD eligible, including fully-integrated care named Fully Integrated Dual Advantage for Intellectual and Developmental Disabilities (FIDA-IDD). Due to challenges surrounding Medicaid overpayments in the developmental disabilities program, there was pressure to reduce funding and improve management.
After years of work by the NY Office for People with Developmental Disabilities (OPWDD) in 2013 legislation was passed authorizing DISCOs, which were required to be “controlled” by non-profit I/DD providers. Stakeholder concerns halted the progress of awarding any contracts on the DISCOs, however, the FIDA-IDD program was approved by CMS in November 2015.
Current Managed Care Program
In 2016, a fresh approach was taken to implement provider-led care coordination in New York. Creating its own unique structure named “Health Home/Care Coordination Organizations” (HH/CCOs). The entities with a minimum of 51% non-profit I/DD providers handle the care coordination for a capitated rate. Effective July 1, 2018, CCO’s began delivering the I/DD Home Health (HH) services that this program has relied on for its’ first two years.
As of February 2020, the OPWDD is serving nearly 120,000 Medicaid enrolled individuals with I/DD. 350 agencies were consolidated into seven regional HH/CCP organizations and are providing services throughout the state. Enrollment was voluntary, but since existing service coordinators were shifted into these new larger regional organizations much of the population moved to the new system quickly.
The goal of the managed care program focused on a person-centered system to better meet individuals’ needs, enhancing care coordination and service plans, improving community-based services, and establishing transparent finding streams. While enrollment has been live since July 2018, it’s still too early to see if it’s fully working. This program is still considered “emerging” and we will continue to monitor results over time.

Both North Carolina and New York have taken their time with the new programs, spending years to get to this point. North Carolina will have to wait a bit longer to see if their approach is successful with COVID-19 delaying the launch. New York is already seeing success, enrolling over 100,000 people. Both programs focus on the whole-person approach, giving individuals options with a regional approach. Time will tell how successful these models can be. In our next blog, we will do a full breakdown of the ten states I/dd managed care programs.
Advocate’s Perspective: With these two programs being some of the newest we’ve covered, it’s obvious that provider-led care is the future of successful managed care programs. Provider-led care offers a greater level of assurance for the consumer and ensures that their needs will be met. There can be drawbacks to this, as we have seen with other states such as Arkansas and Wisconsin that rushed in too quickly. This approach takes time! We are also seeing person-centered care rising to the forefront giving individuals options and more control over their care and overall lifestyle. These approaches offer incredible levels of quality of life.
Onward!
Share This Blog!
Get even more insights on Linkedin & Twitter

About the Author
Fady Sahhar brings over 30 years of senior management experience working with major multinational companies including Sara Lee, Mobil Oil, Tenneco Packaging, Pactiv, Progressive Insurance, Transitions Optical, PPG Industries and Essilor (France).
His corporate responsibilities included new product development, strategic planning, marketing management, and global sales. He has developed a number of global communications networks, launched products in over 45 countries, and managed a number of branded patented products.

About the Co-Author
Mandy Sahhar provides experience in digital marketing, event management, and business development. Her background has allowed her to get in on the ground floor of marketing efforts including website design, content marketing, and trade show planning. Through her modern approach, she focuses on bringing businesses into the new digital age of marketing through unique approaches and focused content creation. With a passion for communications, she can bring a fresh perspective to an ever-changing industry. Mandy has an MBA with a marketing concentration from Canisius College.