How State Medicaid Policies Shape LTSS Environments and Outcomes – Part 2
States with Progressive Medicaid Policies Rated Better in AARP LTSS Scorecard

THE VBP Blog
December 7, 2023 – In the intricate world of healthcare, Long Term Services and Supports (LTSS) stand out as a vital component, especially as our population ages. LTSS encompasses a broad array of services designed to assist individuals who require sustained support to manage their daily lives. As each state navigates its unique challenges and resources, the approach to delivering and funding LTSS varies.
In this blog, we look at what LTSS entails and how different states shape the environment of care and support at home with various policies and programs. This blog focuses particularly on how different states administer these services, the critical role of Medicaid, and the resultant disparities in care and accessibility.
Quick Recap: LTSS 101
Long Term Services and Supports (LTSS) refers to the variety of services include both home health and home care services that enable individuals to live independently and safely when they can no longer perform everyday activities on their own. LTSS can be provided in various settings, such as the individual’s home, a community facility, or institutional environments like nursing homes. These are typically services that people receive for months or even years, which is why they are referred to as long-term care. Medical services typically involve nursing care, medication management, or therapy sessions. On the other hand, non-medical assistance includes help with daily living activities like bathing, dressing, meal preparation, and transportation. The goal of LTSS is to promote autonomy and facilitate community living, where individuals can enjoy a sense of normalcy and participation in their daily lives.
There are various ways to pay for LTSS. Medicare covers up to 100 days of nursing home care, but only if the individual needs skilled services in an inpatient setting and no non-medical services are covered. Medicaid is the primary payer of LTSS and to qualify for that you must meet state-specific eligibility requirements based on income, wealth, and functional limitations. Many individuals do not qualify for Medicaid, so they are forced to pay out of pocket for at-home LTSS services or receive unpaid assistance and care through family and friends.
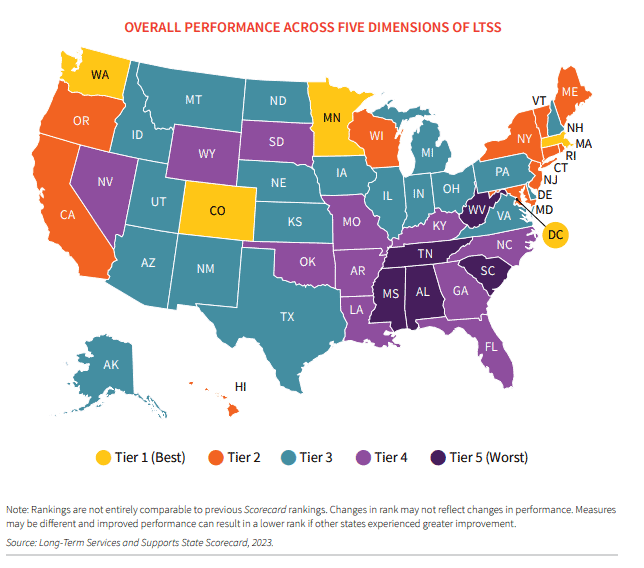
Because states vary on their Medicaid coverage for LTSS, as the 2023 AARP Long-Term Services and Supports (LTSS) State Scorecard shows in the map below, there is a big disparity when it comes to LTSS outcomes and state ranking.
The Pivotal Role of Medicaid in Shaping LTSS
So, how does Medicaid shape the LTSS landscape in states? Simply put, Medicaid is the cornerstone of the Long-Term Services and Supports (LTSS) system in the United States. As the largest payer for LTSS, Medicaid’s policies significantly influence how services are structured, delivered, and accessed. The choices states make in configuring their Medicaid programs have far-reaching implications, not just for the beneficiaries, but for the entire LTSS landscape.
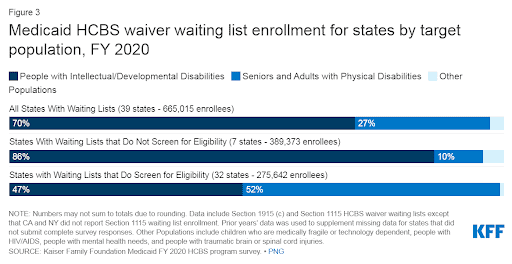
Varied HCBS Environments: State-level policy decisions lead to diverse Home and Community-Based Services (HCBS) environments. Medicaid HCBS can be provided as part of State plan services or through waivers. State plan HCBS include mandatory services (all states must offer them), and optional services (offered at states’ discretion). For example, some states offer generous benefits and have high reimbursement rates that encourage provider participation, while others may have more restrictive policies, impacting the availability and quality of services. A recent KFF brief shows that while all states offer home health services through Medicaid HCBS programs, only 37 offer personal care services. Diving further into that, while the majority of states offer personal care services, who is actually eligible for them also varies. As does the funding for these programs, which impacts overall access to availability of services. States can also cap HCBS waiver enrollment, which creates waiting lists when the number of people in need of services is higher than the number of waiver slots available. There are over 665,000 individuals on waiting lists and as the chart below shows, the majority of these individuals are people with intellectual and development disabilities who need services the most.
These disparities can affect everything from the availability of in-home care to the capacity for innovation in service delivery.
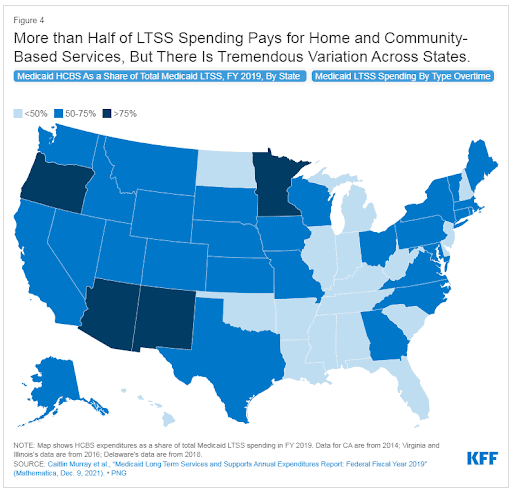
Spectrum of LTSS Coverage: Medicaid’s flexibility allows states to experiment with different models of care and coverage, yet this also leads to unevenness in service provision. The Kaiser Family Foundation (KFF) highlights that Medicaid’s state-specific approach creates a spectrum of LTSS coverage where some states extend broad, comprehensive LTSS benefits, including a wide array of HCBS, while others have narrower coverage, often leading to longer waiting lists for services and less choice for consumers. It’s important to note that when you compare a map of overall performance of LTSS from the AARP scorecard to one that highlights how much a state spends on HCBS through LTSS spending (shown below), the states with higher spending tend to rank higher in overall performance, while states with low HCBS spending rank low in overall performance. This highlights the importance of delivering quality services where individuals want them most, which is often in home and community settings, and not in institutional settings.
Impact on Quality and Access: The structure of Medicaid reimbursement rates and policies around eligibility and scope of services directly affects the quality of and access to LTSS. Higher rates can lead to better quality care as providers are more likely to invest in training and retaining skilled staff. Conversely, lower rates may contribute to workforce shortages and lower quality care, as seen in the workforce challenges facing the LTSS sector. States in the top two tiers all performed better than average on workforce indicators. We are already experiencing a workforce crisis in the healthcare industry, especially in home health and home care. Without this crucial network of caregivers, consumers will not have access to the LTSS services they need. While the workforce shortage is something felt across the country, some states are stepping up to do something about it and those are faring better in terms of LTSS scores. The AARP report found that 20 states had policies in place that require providers receiving Medicaid reimbursement to pass through either a certain dollar amount
or percentage of reimbursements to direct care workers. States like California have set minimum wage requirements for healthcare workers. Other states like Washington have allocated funds in the budget to target wage increases. Both states are in the top two tiers for LTSS and score well in workforce indicators.
Family Caregiver Support: State Medicaid policies also influence support for family caregivers, who are an integral part of the LTSS system. Some states have developed Medicaid waiver programs that recognize and compensate family caregivers, whereas others have yet to establish such supports, placing the full burden of care on families without formal recognition or assistance. The report found that prioritizing family caregivers is essential. Thre are over 48 million family caregivers that provide more than $600 billion in unpaid care. These individuals need help and the states that have policies in place to support caregivers through CARE Act legislation, paid sick leave, tax credits and other mechanisms to address the family caregivers’ health and financial needs, tended to have better overall long-term services and support systems. As the aging population grows, so will the next for LTSS services. With many home health agencies and home care agencies already tapped and being forced to reject new referrals, maintaining the support network of family caregivers is essential for keeping individuals living independently and comfortably at home.
Advocates Perspective
Each state’s approach to LTSS is shaped by its unique policy decisions, particularly within Medicaid. State-specific Medicaid policies play a defining role in the structuring of LTSS, significantly influencing the sustainability of care models, the support of caregivers, and the well-being of recipients. And as such, it creates much variability on outcomes and satisfaction of consumers. While the diversity in state policies can fuel creativity and lead to model programs, we must ensure that every individual who requires long-term care can receive it regardless of where they live. But doing so will likely require some sort of intervention from the federal government, as right now, states are left to their own demise when it comes to LTSS, and many are not making decisions that support quality of care and access to services that individuals need.
Onward!
Share This Blog!
Get even more insights on Linkedin & Twitter

About the Author
Fady Sahhar brings over 30 years of senior management experience working with major multinational companies including Sara Lee, Mobil Oil, Tenneco Packaging, Pactiv, Progressive Insurance, Transitions Optical, PPG Industries and Essilor (France).
His corporate responsibilities included new product development, strategic planning, marketing management, and global sales. He has developed a number of global communications networks, launched products in over 45 countries, and managed a number of branded patented products.

About the Co-Author
Mandy Sahhar provides experience in digital marketing, event management, and business development. Her background has allowed her to get in on the ground floor of marketing efforts including website design, content marketing, and trade show planning. Through her modern approach, she focuses on bringing businesses into the new digital age of marketing through unique approaches and focused content creation. With a passion for communications, she can bring a fresh perspective to an ever-changing industry. Mandy has an MBA with a marketing concentration from Canisius College.
