Expanding PACE - Revolutionizing Care for the Elderly
Ohio to Expand PACE to six new counties as the program gains steam across the country

THE VBP Blog
June 15, 2023 – Our elderly population deserves a comprehensive healthcare system that addresses their multifaceted needs. That is what the Program of All-Inclusive Care for the Elderly (PACE) aims to do.
PACE is a Medicare and Medicaid program that allows our aging population to meet their needs in the community, instead of going to a nursing home or care facility. In this blog post, we will delve into the heart of PACE, exploring its services and benefits, and its expansive trajectory across the United States.
Who Qualifies for PACE?
PACE is a unique care model that integrates a comprehensive suite of health services for elderly individuals. Those who join PACE get a team of healthcare professionals who coordinate your care in the community. To be eligible for PACE, you must be at least 55, need a nursing home-level of care, and are able to safely live in the community with the help of PACE. You must also live in the service area of a PACE organization.
Medicare eligibility requires participants to be a US citizen or legal resident for at least 5 years, at least 65 years of age, or disabled. Medicaid eligibility is not as straightforward as it varies by each state. Typically, seniors and disabled persons are eligible for long-term care Medicaid in 2023 if they have income under 300% of the Federal Benefit Rate, have assets valued at $2,000 or less (excluding the primary home), or require a Nursing Home Level of Care. You don’t have to have Medicare or Medicaid to qualify. Those who are not Medicaid-eligible can elect to pay the monthly private pay portion for the long-term care Medicaid benefit of PACE, and the monthly premium for prescription drug. This typically adds up to $4,000 to $5,000 per month, which can be burdensome to most consumers.
What Services are Offered Through PACE?
So, what services does PACE offer? Overall, PACE addresses the medical, social, and personal care needs of seniors. It provides wrap-around care and a patient-centered approach that prizes flexibility and responsiveness. Services range from adult day care, dentistry, prescription medicines, emergency services, home care, laboratory services, nutritional counseling, preventative care, and social work counseling. But it doesn’t stop there. PACE also steps into the everyday life of its participants, offering meal assistance, transportation, and caregiver support.
The benefits of PACE are profound. By fostering an environment of coordinated care, PACE not only promotes a higher quality of life but also reduces hospitalizations and ER visits. One of the major goals of the program is to prevent or delay any unnecessary nursing home admissions, and through a unique mix of home and community-based service and supports, it allows seniors to remain in their homes and community, enhancing their independence.
The Expanding Horizon of PACE
Due to the level of care and benefits that PACE provides, it is a highly sought after program. However, as great as the PACE program is, it is not available nationwide. As of February 2023, PACE operates in the District of Columbia and 32 states. In total, there are 151 PACE Programs across the country. Yet, as the map below shows, there’s still room for growth.
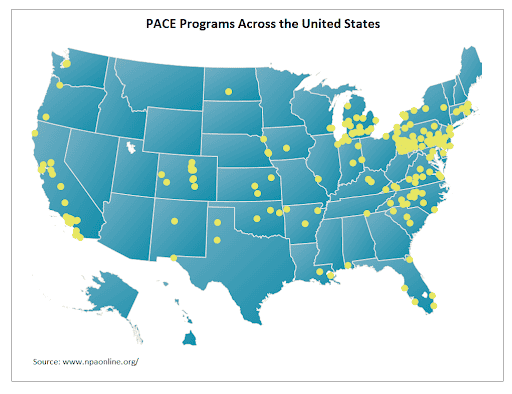
The issue, as seen in the map above, is that even states that have PACE programs often don’t have enough to cover the entire population of the state. One-fourth of older Americans live in one of three states: California, Florida, and Texas. As you can see, while California has PACE programs spread out across the state, Florida, and certainly Texas, do not have adequate coverage. Seven other states—Georgia, Illinois, Michigan, New York, North Carolina, Ohio, and Pennsylvania—account for roughly another quarter of the 65 and older population. While Pennsylvania has an abundance of PACE organizations that allow consumers more choice, two of those states do not even have PACE programs. This not only means that consumers might not have access to a PACE program, but those who do, have little to no choice on their providers. Program enrollees can only see providers that participate in PACE, which can be very limited, and in some cases, leave consumers no choice or options if they do not like the available provider at the PACE center.
As the elderly population in the United States continues to grow, the need for integrated care programs like PACE becomes increasingly vital to allow individuals to remain living comfortably and independently at home. Recognizing this, the expansion of PACE programs has been ramped up nationwide.
Ohio recently announced plans to expand PACE to six new counties. Currently, Ohio only has one PACE site, but the state released an RFP to serve new sites in Franklin, Hamilton, Montgomery, Lorain, Lucas, and Summit counties. In addition to those, the state will also consider proposals for an additional rural county. This is important as we look to health equity as many of these programs are concentrated in more densely populated areas, leaving rural communities out of the mix.
Despite its tangible benefits, several challenges lie in the path of PACE expansion. These include stringent eligibility criteria, infrastructure demands, and funding constraints. Addressing these obstacles head-on and capitalizing on regulatory flexibility can help to broaden the reach of PACE.
Looking Ahead
PACE has proved to be an effective value-based payment model for providing care to Medicare and Medicare-Medicaid dual-eligible patients relative to fee-for-service comparison groups. Participants in PACE programs have reported better care management, a reduction in hospitalizations, and tended to live longer than patients cared for in nursing homes. This not only reduces healthcare costs, but it also mitigates health disparities. Analysis by the state of Oklahoma showed that for every 100 individuals served by a PACE program, the state saves over $1.2 million per year. There are also other studies across over 20 years of data that show a strong association between PACE enrollment and reduced hospitalizations.
One thing we don’t have much of is data regarding consumer satisfaction. Some early studies show that there is a low disenrollment rate for PACE (7%), which indicates that consumers are satisfied with the care they receive. A recent 2021 study of the McGregor PACE Program in Ohio, shows that 97% of participants also have a high level of satisfaction with the program. Another study in New York from 2022 shows that 96% of family members are satisfied with PACE support and 97.5% would recommend PACE. A Pennsylvania study also shows that members rarely unenroll from the program, which typically means they are satisfied with the care they are receiving. While these are one off studies, it is encouraging to see consumer satisfaction at the state level. However, all-encompassing national data would be able to provide a better overall picture of PACE.
With its all-encompassing and patient-centered approach, PACE provides our elderly population with the much-needed care and support they deserve while ensuring their dignity and independence. But that doesn’t mean that it comes without some concerns. As mentioned before, consumers have little choice as they must see a provider that participates in PACE, and that can be limited. They also have a limited selection of services, and they must all be received at the same site, with no alternatives. In theory, PACE is an integrated care platform that allows individuals to remain living independently at home, but with expansion, consumers need to be well-educated on the potential risks.
Another risk is that in the case of a catastrophic health event, the PACE provider directs all care. This can mean increased care coordination, but if consumers are unhappy with their provider, they may not want them to be the ones to direct care.
As we look at the future, the expansion of PACE provides a compelling template for nationwide implementation. With sustained commitment and innovative solutions, PACE can pave the way for a healthier future for our elderly population. It can also reduce healthcare costs for a nation that has some of the highest healthcare costs in the world. The journey to optimal health outcomes and reduced health disparities for our aging population is far from over, but with PACE, we’re at least on the right path.
Advocates Perspective
PACE is a unique program with a plethora of benefits for those eligible. However, while 32 states are offering PACE, only just over 40% of individuals living within a supportive PACE state have access to a PACE program. And those that do have access to a PACE program, may have limited options on providers. As PACE expands to allow our aging population and people with disabilities to take advantage of the services and coordinated care offered through the program, expansion needs to be carefully planned. We’ve seen studies that show PACE programs can reduce healthcare costs and lower health disparities, but consumer choice and quality of care needs to be at the forefront. Increasingly, PACE is being expanded through insurance companies or for-profit companies. That is okay if these are the organizations that have the means to expand PACE across the country, but there needs to be some guidelines on services required, and how to educate consumers on what they will actually be getting through the PACE program in terms of choice. While the PACE program is a way to address disparities while effectively incorporating value-based care into senior care, there needs to be funding and proper development partners to ensure that quality of care and consumer choice remains the focus of PACE.
Onward!
Share This Blog!
Get even more insights on Linkedin & Twitter

About the Author
Fady Sahhar brings over 30 years of senior management experience working with major multinational companies including Sara Lee, Mobil Oil, Tenneco Packaging, Pactiv, Progressive Insurance, Transitions Optical, PPG Industries and Essilor (France).
His corporate responsibilities included new product development, strategic planning, marketing management, and global sales. He has developed a number of global communications networks, launched products in over 45 countries, and managed a number of branded patented products.

About the Co-Author
Mandy Sahhar provides experience in digital marketing, event management, and business development. Her background has allowed her to get in on the ground floor of marketing efforts including website design, content marketing, and trade show planning. Through her modern approach, she focuses on bringing businesses into the new digital age of marketing through unique approaches and focused content creation. With a passion for communications, she can bring a fresh perspective to an ever-changing industry. Mandy has an MBA with a marketing concentration from Canisius College.