Health Equity to Become Part of the VBP Future
CMMI Director says creating a health equity plan is likely to be a requirement to participate in VBP models
THE VBP Blog

In our last blog, we took a deep look into health equity – what it is and how it impacts health outcomes. In this blog, part two of the two-part series on health equity, we are going to look at how health equity is primed to become part of the value-based payments (VBP) future.
In fact, organizations that are interested in participating in value-based care payment models should start focusing on the creation of a health equity plan. At least, that’s what Center for Medicare and Medicaid Innovation (CMMI) Director Liz Fowler suggested.
“You can expect future innovation center models to have features like ACO REACH, like requirements for health equity plans,” Fowler stated during AHIP’s 2022 National Conference on Health Policy and Government Health Programs.
The statement may seem a bit farfetched, but recent announcements have shown that the focus on health equity is very real. This includes the recent inclusion of requiring a health equity plan for accountable care organizations (ACOs) interested in participating in the revamped ACO REACH model.
The ACO REACH model, set to replace Direct Contracting in 2023, includes several requirements for improving health equity. This includes the creation of a health equity plan, an adjustment to the benchmarks to better reflect health equity, and adjusting payments to incentivize better care coordination in underserved areas. ACO REACH is the first model to require a health equity plan, but this is just the tip of the ice burg.
CMS is Pushing Prioritization of Health Equity
Recently, CMS has made strides to advance health equity through various initiatives. In April 2022, the agency released the CMS Framework for Health Equity 2022-2032. This is an action plan that will be used to address health disparities across every program and community that CMS touches.
“Health equity will be embedded within the DNA of CMS and serve as the lens through which we view all of our work…We will not stop until every person has a fair and just opportunity to attain their optimal health,” said CMS Administrator Chiquita Brooks-LaSure.
With CMS acting as the largest provider of health insurance in the county, it is paramount that the roughly 170 million individuals supported by CMS programs get the coverage and care that they need. To achieve these goals, CMS has laid out a framework for health equity priorities. As the chart below shows, there are five priorities in the health equity framework.
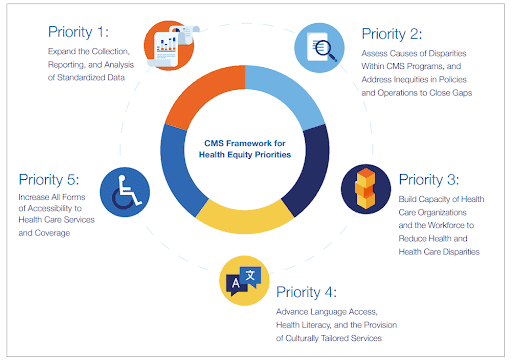
This framework is consistent with the Department of Health and Human Services’ Healthy People 2030 Framework, as well as the Healthy People 2000 Framework that first incorporated health equity as a guiding objective. Through the framework, CMS will look to shape their programs as they work to address avoidable inequalities and eliminate health and health care disparities.
How CMS progresses is something that we will certainly keep an eye on as it will have a big impact on those in the LTSS and IDD communities. A recent study shows that those with disabilities face many challenges to not only achieving optimal health but also accessing high-quality care. CDC data from 2019 also shows that people with disabilities have less access to health care, have more depression and anxiety, and are less physically active when compared to people without disabilities. Healthy equity plans must address the IDD and LTSS communities to ensure quality care for all.
Innovation Center Launches Refresh with Health Equity at the Forefront
The CMS Innovation Center also recently announced a strategy refresh that includes advancing health equity as one of the five main objectives. The CMS Innovation Center was established in 2010 through the Affordable Care Act. The agency’s overarching goal was to transition the healthcare industry to value-based care through the development, testing, and analysis of new payment models. Over the last 10 years, CMMI has tested over 50 models and learned a lot along the way
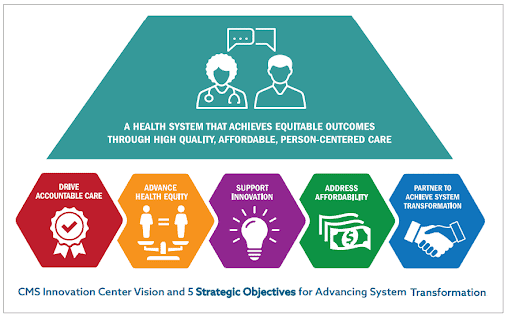
The chart above shows the objectives that have been derived through that decade of testing and learning. These five goals will drive the Innovation Center’s work, guiding the creation of VBP models and priorities for years to come, though the ultimate goal of expanding successful models that reduce program costs and improve quality and outcomes for Medicare and Medicaid beneficiaries remains.
What’s unique about CMMI’s strategy refresh white paper, is that goals for both beneficiaries and providers are considered. As we’ve discussed in the past, it is always important to consider and include all stakeholders in the process of developing value-based payment models and health equity plans.
These health equity initiatives are also being driven by policymakers. The John Lewis Equality in Medicare and Medicaid Treatment Act was recently introduced by Rep. Terri Sewell, D-Alabama. The legislation aims to advance health equity in the work of CMMI by requiring the agency to rethink how it approaches value-based payment models.
The bill specifically calls for the creation of a new social determinants of health model that highlights the “health conditions of those dually eligible for Medicaid and Medicare, behavioral health and maternal mortality,” while also requiring the participation of experts on health disparities in the review and evaluation of any new CMMI models. In addition, new VBP models must also consider how people of color, women, and those in rural areas will be impacted when it comes to health equity, cost, and quality of care.
The bill has support from various organizations, including the National Association of Orthopaedic Nurses, the National Black Nurses Association, The Root Cause Coalition, and the Academy of Medical-Surgical Nurses, among others. The bicameral legislation was recently introduced in the House of Representatives and was referred to various committees in May for consideration.
Advocates Perspective
It is encouraging to see that health equity is being brought to the forefront by CMS, CMMI, and policymakers alike. We know the importance of every individual being able to achieve their full health potential regardless of socially determined circumstances outside of their control. However, as the shift to VBP and the creation of health equity plans continues, it is essential to get it right and that means stakeholders in the process. This can be a promising advancement for those in the IDD and LTSS communities, but only if their specific needs and challenges are considered throughout the process.
Onward!
Share This Blog!
Get even more insights on Linkedin & Twitter

About the Author
Fady Sahhar brings over 30 years of senior management experience working with major multinational companies including Sara Lee, Mobil Oil, Tenneco Packaging, Pactiv, Progressive Insurance, Transitions Optical, PPG Industries and Essilor (France).
His corporate responsibilities included new product development, strategic planning, marketing management, and global sales. He has developed a number of global communications networks, launched products in over 45 countries, and managed a number of branded patented products.

About the Co-Author
Mandy Sahhar provides experience in digital marketing, event management, and business development. Her background has allowed her to get in on the ground floor of marketing efforts including website design, content marketing, and trade show planning. Through her modern approach, she focuses on bringing businesses into the new digital age of marketing through unique approaches and focused content creation. With a passion for communications, she can bring a fresh perspective to an ever-changing industry. Mandy has an MBA with a marketing concentration from Canisius College.