Local Engagement in IDD Managed Care in Arizona and Michigan
THE VBP Blog
[5/26/2020] –
As promised, this blog will examine the last 4 states that offer I/DD managed care programs to their consumers.
This week, we take a look at Arizona and Michigan. Arizona built a completely different structure than we have seen before with a state-run Division of Developmental Disabilities as the managing entity. Michigan’s managed care program is similar to that of North Carolina, focusing on county-based programs. These two contrasting styles have both found success and both have created unique solutions to manage the I/DD and MLTSS population.

Arizona's Managed Care Program
Arizona’s Long-Term Care System (ALTCS) was established in 1998 for the management of Long-Term Services and Support (LTSS), working with 66,669 consumers as of March 1, 2020. Their Medicaid program is designed to help fixed income seniors and other disabled individuals afford the care they need. For people with I/DD, the Arizona Division of Developmental Disabilities (DDD) serves as the managing entity under a capitated rate through a contract with Arizona Health Care Cost Containment System (AHCCCS). According to the azahcccs.gov website, the capitated monthly rate through 9/30/2020 for a regular DDD consumer is $4840.31, up from $3628.21 under the 2018 contract.
Since Arizona started their Medicaid program later than other states (1982) and is primarily relying on state dollars, they learned from states that already had a Medicaid program and avoided some of the institutional bias. With their focus on developmental disabilities and more specifically HCBS, they have emphasized serving individuals in family homes.
96.6% of Medicaid LTSS dollars for people with I/DD in home & community settings in 2015
The results? In 2015, 96.6% of all Medicaid LTSS dollars for people with I/DD were delivered in home and community-based settings. The structure presented challenges such as providers facing low reimbursement rates, little to no rate growth, and an administration that sets rates below cost
A New Managed Care Program Contract in 2019
In October of 2019, a new 3-year contract went into effect with MCOs Mercy Care and UnitedHealthcare Community Plan (UHCCP). The new integrated plans are intended to allow better coordination of services and to make the system easier. According to their state website, “these DDD Health Plans will offer eligible members physical and behavioral health services, Children’s Rehabilitative Services (CRS) and limited long term services and supports (LTSS): nursing facilities, emergency alert system services, and habilitative physical therapy for members age twenty-one (21) and over. All other LTSS and Support Coordination will be provided by DDD. This model will enhance care treatment between providers and improve member health.”
We will return to evaluate the true effectiveness of this integrated model as soon as there is sufficient data to do so.
Michigan's Managed Care Program
Michigan’s structure is the only one that operates like North Carolina with county-based Community Mental Health Services Programs (CMHSPs) and local Prepaid Inpatient Health Plans (PIHPs). This managed care structure is offered through the 1915(b) Managed Specialty Services and Supports Waiver and the 1915(c) Habilitation Supports Waiver. The Medicaid funding for behavioral health and I/DD services is provided by the Michigan Department of Health and Human Services (MDHHS) to 10 PIHPs throughout the state. Three PIHPs are also structured as CMHSPs with the total CMHSPs being 46.
As with most other states, the main goals of the managed PIHP model are freedom, community, accountability, and efficiency. The state also worked with the stakeholders to create a program that focused on HCBS, without following in the steps other states had taken with traditional MCOs or privatization. This approach has its downfalls: with multiple counties across the state having different procedures, quality expectations, billing, etc. there are going to be issues. It also has benefits, however, with person-centered planning at the forefront.
BOLD Council
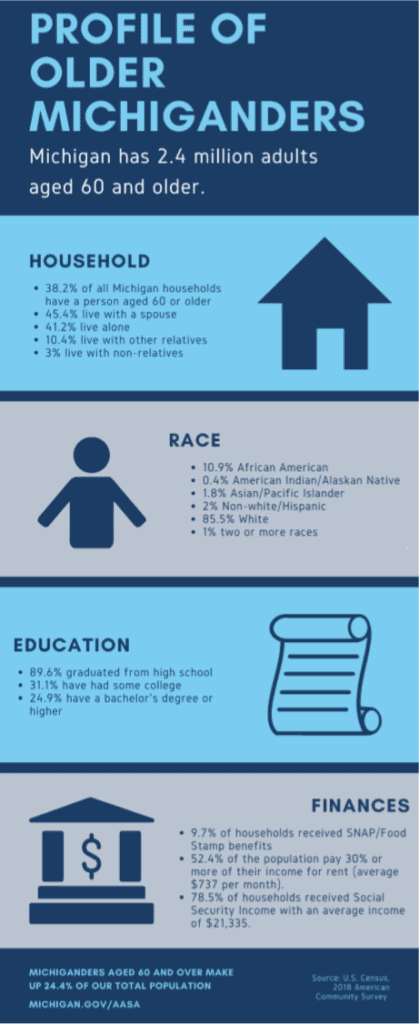
As of 2019, Michigan has 2.4 million adults ages 60 or older. The state has created the BOLD Council (Building Options for LTSS Decision-making), a state-level collaborative tasked to improve LTSS and integrate access to services. BOLD works with the Medical Services Administration, Behavioral Health and Developmental Disabilities, Rehabilitation, and Department of Licensing Services.
We see some rare commonalities between the two states we covered here. Both states include programs for the I/DD and LTSS communities and both have a significant role for state or local government. Arizona’s capitated structure has found success as well as Michigan’s regional PIHP design.
Both of these programs have flaws: Arizona’s providers feel shortchanged with rates set low and Michigan’s counties have differing expectations. Having the state or local government involved creates inconsistencies that make the program less reliable. As we’ve seen with other states, both have found some version of success as well and are continuing to morph.
Advocate's Perspective
One of the big takeaways from this article is Arizona’s 96.6% of Medicaid LTSS dollars going to home and community care. Their program has been substantially effective in getting money to keep consumers at home. If your state has a local-based structure or doesn’t have a program yet, getting involved in your local or state government can have a large bearing on how your business is impacted. Understanding what policies are being laid out as decisions are being made will give you an opportunity to plan well in advance. Also, having service coordination activities separated from the MCO gives providers an opportunity to influence how consumers are treated within a managed care system.
Onward!
Fady Sahhar & Mandy Sahhar
Share This Blog!
Get even more insights on Linkedin & Twitter

About the Author
Fady Sahhar brings over 30 years of senior management experience working with major multinational companies including Sara Lee, Mobil Oil, Tenneco Packaging, Pactiv, Progressive Insurance, Transitions Optical, PPG Industries and Essilor (France).
His corporate responsibilities included new product development, strategic planning, marketing management, and global sales. He has developed a number of global communications networks, launched products in over 45 countries, and managed a number of branded patented products.

About the Co-Author
Mandy Sahhar provides experience in digital marketing, event management, and business development. Her background has allowed her to get in on the ground floor of marketing efforts including website design, content marketing, and trade show planning. Through her modern approach, she focuses on bringing businesses into the new digital age of marketing through unique approaches and focused content creation. With a passion for communications, she can bring a fresh perspective to an ever-changing industry. Mandy has an MBA with a marketing concentration from Canisius College.


