Let’s Jump Back in to Managed Care in I/DD
THE VBP Blog
[5/14/2020] – For the past 8 months, we have touched on managed care in the individuals with intellectual and developmental disabilities (I/DD) population. While the world has been coping with COVID-19, this expansion of managed care has not slowed down.

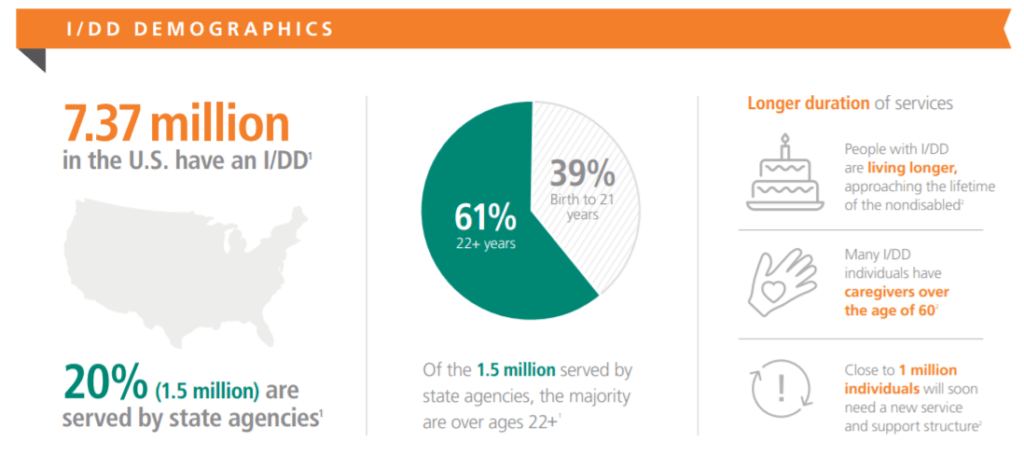
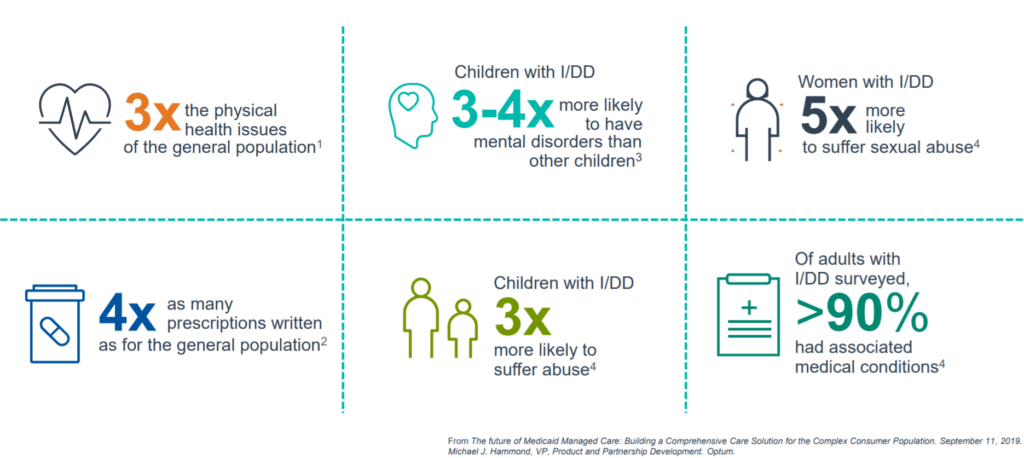
With the estimated 1.5 million Medicaid consumers with an I/DD, over 358,500 consumers with I/DD were enrolled in a managed long-term services and supports (MLTSS) program over 10 states as of May of 2020. This means approximately 2.1% of the total Medicaid population and 25.4% of I/DD consumers enrolled in a Medicaid program. This population has 45% with three or more chronic conditions and 35% always have a mental illness. As you can see in the Optum graphic, members of this group also live longer, are in need of a care giver, and often need to add more services.
Managed Care Quality Measures
In September 2019, we attended the Rehabilitation and Community Providers Association (RCPA) Conference in Hershey, PA and sat in on an incredible session by Joan Martin, Donna Martin, and Alissa Halperin. From that talk, we wrote two blogs outlining Quality Measures in the I/DD and MLTSS communities. In a nutshell, the need for lifelong care, high levels of care, and MCOs’ lack of experience with these communities have made the transition to managed care difficult. We broke down the different quality measures that are being used to ensure value-based care from the National Quality Forum, the Council of Quality and Leadership, and the National Core Indicators. All revealed that there are many ways for your business to become informed of the changes you can make to be ready for managed care.
Managed Care State Models
Individuals with I/DD are unique, which is why managed care has been a difficult task for most states. On average, they need 4x as many prescriptions and have 2x the physical health issues of the general population. These factors create challenges – particularly in case management – that states are still trying to figure out.
We have taken a look at six of the ten states so far and have broken down the successful and less successful models. We came to a few conclusions as well:
- Time matters – the states that allowed themselves more time in development have much more successful programs
- Case management – in states that focused on this factor, consumers were ultimately taken care of quickly and cost effectively; in states that under-prioritized case management, chaos reigned
- Multi-state MCO’s aren’t always the answer – some states found success with multi-state MCO’s but others were deemed just as successful using alternate models
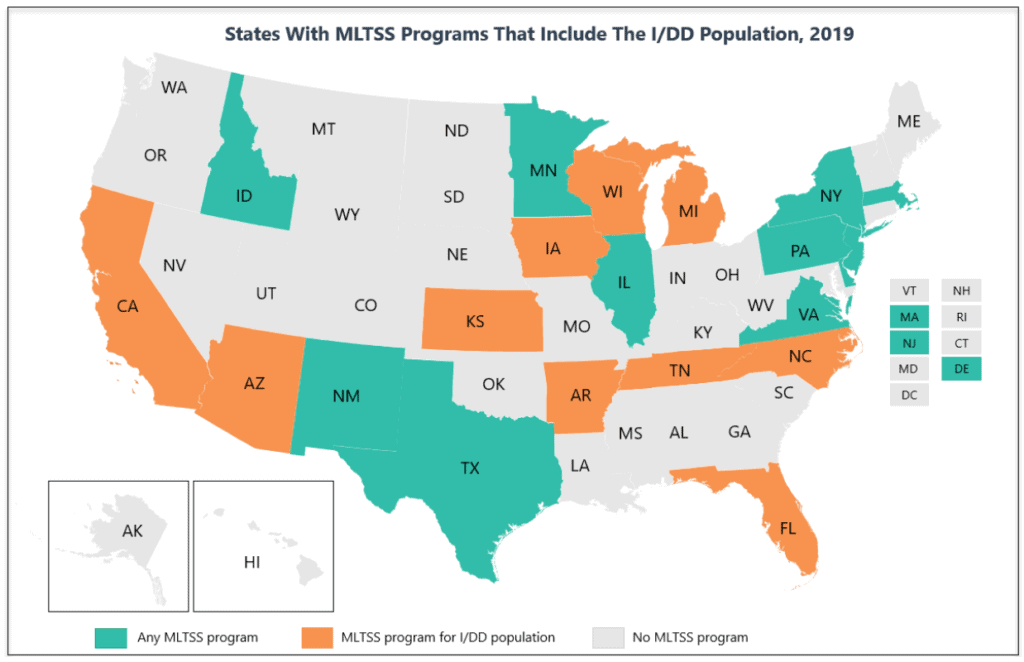
There are also 12 states – Delaware, Hawaii, Illinois, Massachusetts, Minnesota, New Mexico, New York, Pennsylvania, Rhode Island, Tennessee, Texas, and Virginia – that currently exclude their I/DD population from enrolling in MLTSS. They may change their tune soon as the market continues to shift and outcomes are directly connected to payments. With the I/DD community served by Medicaid, Medicare, and commercial models, there are opportunities for diversity in how states approach managed care.
Over the next few weeks, we will take deeper looks into the final four states with managed care I/DD programs: New York, Arizona, Michigan, and North Carolina. These states each have unique approaches with Michigan and North Carolina operating on a local-county based Prepaid Inpatient Health Plans and Arizona using the state Division of Developmental Disabilities as their managing entities. We will cut through the noise and give you facts on exactly what is and isn’t working.
Advocate's Perspective
Keep focusing on quality and taking care of your consumer first. Quality includes protecting consumer protections for our consumers that we have fought hard for. It also means technology and innovation, such as telehealth changes that are consistently improving how care is done. Finally, quality means consumer engagement and creating brand loyalty that will set you apart from your competitors.
Onward!
Fady Sahhar & Mandy Sahhar
Share This Blog!
Get even more insights on Linkedin & Twitter

About the Author
Fady Sahhar brings over 30 years of senior management experience working with major multinational companies including Sara Lee, Mobil Oil, Tenneco Packaging, Pactiv, Progressive Insurance, Transitions Optical, PPG Industries and Essilor (France).
His corporate responsibilities included new product development, strategic planning, marketing management, and global sales. He has developed a number of global communications networks, launched products in over 45 countries, and managed a number of branded patented products.

About the Co-Author
Mandy Sahhar provides experience in digital marketing, event management, and business development. Her background has allowed her to get in on the ground floor of marketing efforts including website design, content marketing, and trade show planning. Through her modern approach, she focuses on bringing businesses into the new digital age of marketing through unique approaches and focused content creation. With a passion for communications, she can bring a fresh perspective to an ever-changing industry. Mandy has an MBA with a marketing concentration from Canisius College.

