How New York is Using Value-Based Payment to Transform Managed Long-Term Care Plans
New York Leads the Way in Integrating Quality with Cost-Effectiveness

THE VBP Blog
October 26, 2023 – In recent years, health care payment models have been in a state of evolution, shifting focus from volume-based systems like fee-for-service to models that prioritize value. New York State, always a frontrunner in health reform, is taking the initiative to blend this modern approach with their managed long-term care (MLTC) plans.
The introduction of value-based payment for MLTC plans promises not just enhanced quality of care but also a more efficient expenditure of resources. But the transformation poses the question: How will this merger impact patients, providers, and the overall healthcare landscape in New York? In this blog, we are going to take a close look at managed long-term care and explore the implications of New York’s progressive steps towards integrating value-based payments.
What is Managed Long Term Care?
Managed Long Term Care (MLTC) is a system tailored to assist individuals who are chronically ill or have disabilities that put them at risk of nursing home placement. It provides these individuals with long-term health and social services to maintain their quality of life while they remain at home and in their communities. These services covered by managed long-term care plans include things like:
- Home care (including personal care, home health aide,
- Consumer Directed Personal Assistance
- Adult day care
- Private duty nursing
- Physical/Occupational/Speech therapy
- Transportation to medical appointments
- Home delivered meals
- Medical equipment and supplies
- Hearing aids and audiology
- Eyeglasses and vision care
- Dental care
- Podiatry
- Temporary nursing home stays
In New York, managed long-term care plans are mandatory for those who require health and social services for more than 120 days that are dual eligible (eligible for both Medicaid and Medicare) and over 21 years. Enrollment in a MLTC plan is voluntary for individuals that are dual eligible and are 18 through 21 years of age and need community based long term care services for more than 120 days and assessed as nursing home eligible, or those who are non-dual eligible and over 18 years of age and are assessed as nursing home eligible.
The overarching aim of MLTC is to enable enrollees to remain in their homes and communities as opposed to institutional settings. Managed long-term care plans manage, coordinate, and make payments for services on behalf of the enrollee. By consolidating the services under a singular plan, MLTC optimizes the care individuals receive, ensuring that it’s not only comprehensive but also customized to the unique needs of each enrollee.
New York's Transition to Value-Based Payment for Managed Long Term Care Plans
The healthcare landscape is constantly evolving, with a clear shift towards prioritizing quality over quantity. New York State is looking to become an industry leader, and even has a Value-Based Payment Roadmap that is consistently updated. This came about when CMS approved New York’s 1115 waiver demonstration to implement the Delivery System Reform Incentive Payment (DSRIP) program in 2015. Since then, NY has worked with CMS to align its efforts with the U.S. Department of Health and Human Services (HHS) on value-based purchasing and alternative payment models (APMs). Through the roadmap, New York outlined how it would achieve transitioning at least 80% of all Medicaid managed care payments into value-based payment arrangements.
As the roadmap laid out, New York integrated value-based payments into its MLTC plans to align with its goal of creating a healthcare system where providers are incentivized to deliver high-quality, efficient care, rather than simply being compensated for the volume of services rendered. The shift to VBP in the MLTC framework comes in response to the realization that the fee-for-service model might not always result in the best outcomes for patients. Under the traditional fee-for-service system, providers receive payment for each service they perform, and the outcome bears no weight. Under the VBP model, financial rewards and penalties are tied to the quality of care provided, ensuring a more outcome-focused approach.
To facilitate this shift, New York has set up a tiered VBP system for MLTC providers. Depending on the level of risk providers are willing to assume, they can opt for varying degrees of reward potential. There are three contracting levels as shown in the chart below.
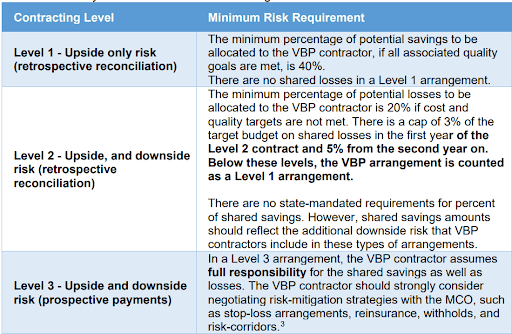
The state does not mandate a specific shared savings/losses distribution methodology, but plans must specify the level of risk and potential shared savings, as well as potential shared losses in the contracts and they must match the definitions provided above.
New York is also taking a unique approach in how social determinants of health (SDOH) are incorporated. For plans choosing Level 2 or Level 3 agreements, they must implement at least one social determinant of health intervention. The SDOH intervention must align with one of the key domains, which include:
- Housing instability
- Food insecurity
- Transportation problems
- Interpersonal safety and toxic stress
- Health literacy and education
- Economic instability
We are seeing more and more states include social determinants of health in the requirements for managed care plans, which is encouraging as these non-medical health needs have a big impact on health outcomes. New York is taking things a step further by using the Pending 1115 waiver to encourage MCOs into more sophisticated contracting arrangements that fund the integration with social care whether through accurate use of Z codes or from collected data. Screening for and addressing these needs can provide a more holistic approach to healthcare by addressing the underlying social factors that influence health outcomes.
What’s also a promising sign for New York’s VBP for managed long term care plans is that the state addressed the Medicaid program with a holistic approach. They went all-in on the transition for MLTC plans, rather than utilizing pilots or a piecemeal approach. While the transition to VBP is not without its challenges, the state offers guidance, resources, and tools to assist providers in this transition, emphasizing collaboration and shared learning.
Why States Should Adopt Value-Based Payment in Medicaid Managed Long-Term Services and Supports
We see that New York is at the forefront of utilizing value-based payments for managed long-term care, but they are not alone. Many states Medicaid programs are looking to transition how they pay providers for long-term services and supports (LTSS) to improve the quality and cost effectiveness of their programs. In fact, over half of states across the country contract with managed care plans to cover LTSS. That is because there are many benefits, including:
Improving Care Quality and Patient Outcomes: Traditional fee-for-service models incentivize the quantity of services over quality. By adopting value-based payments, with carefully selected quality measures, states can instead emphasize the importance of holistic, effective care. Under VBP, providers are rewarded for achieving better health outcomes, reducing hospital readmissions, and enhancing patient experiences. This results in improved patient-centered care that can lead to healthier beneficiaries in the long run.
Cost-Effectiveness and Sustainability: Spiraling healthcare costs are a significant concern for most states. Implementing value-based payment models within MLTSS can lead to significant cost savings. By rewarding providers for efficient, effective care, states can ensure that funds are utilized optimally, reducing wastage and redundancies. Over time, this not only stabilizes Medicaid budgets but also makes the overall system more sustainable.
Encouraging Provider Innovation: One of the notable benefits of value-based payments is that it encourages providers to innovate. Since the focus is on outcomes, healthcare providers are motivated to explore unique, effective strategies for care delivery. This can include harnessing technology, interdisciplinary collaborations, or implementing evidence-based interventions.
Enhanced Data Utilization: The VBP model necessitates robust data analytics to monitor and assess provider performance. As states transition to this model, plans need to invest in advanced health technology and data systems. This can lead to a more informed understanding of patient needs, as well as better collaboration and communication amongst providers and care coordinators.
Risk Management: The VBP model, by design, distributes risk among providers. This ensures that there’s shared accountability. States like New York employ a tiered VBP system that allows providers to select the level of risk they are willing to assume, thus ensuring a more balanced and managed approach to risk-taking. It also allows plans and providers to get acclimated to new VBP models without assuming the maximum amount of risk upfront. The hope is that as time goes by, plans will move down the VBP continuum to assume more risk.
As you can see, the adoption of Value-Based Payment systems in Medicaid Managed Long-Term Services and Supports reflects a broader trend towards making the U.S. healthcare system more proactive, coordinated, and sustainable. By incentivizing outcomes rather than services rendered, states can ensure that beneficiaries in LTSS and long-term care plans receive the best possible care while simultaneously safeguarding the long-term viability of their Medicaid programs.
Advocates Perspective
States like New York, with their forward-thinking approaches, have been instrumental in showcasing the potential of value-based payments in the healthcare system. While New York took a holistic, all-in approach, the state allowed plans to choose their level of risk, which provided some additional comfort as the transition occurred. The journey to fully realizing the potential of VBP is still underway, and it necessitates collaboration from all stakeholders – from state agencies to care providers, and from patients to technology partners. Yet, the initial results and the drive from states signal a promising future for Medicaid beneficiaries, ensuring they receive the care they deserve in a system that continually evolves to meet their needs. As more states adopt and refine VBP models within MLTSS, we are encouraged to see the U.S. shifting to a system that puts patient well-being at the forefront.
Onward!
Share This Blog!
Get even more insights on Linkedin & Twitter

About the Author
Fady Sahhar brings over 30 years of senior management experience working with major multinational companies including Sara Lee, Mobil Oil, Tenneco Packaging, Pactiv, Progressive Insurance, Transitions Optical, PPG Industries and Essilor (France).
His corporate responsibilities included new product development, strategic planning, marketing management, and global sales. He has developed a number of global communications networks, launched products in over 45 countries, and managed a number of branded patented products.

About the Co-Author
Mandy Sahhar provides experience in digital marketing, event management, and business development. Her background has allowed her to get in on the ground floor of marketing efforts including website design, content marketing, and trade show planning. Through her modern approach, she focuses on bringing businesses into the new digital age of marketing through unique approaches and focused content creation. With a passion for communications, she can bring a fresh perspective to an ever-changing industry. Mandy has an MBA with a marketing concentration from Canisius College.
