Behavioral Health Series: The Role of Managed Care in Tackling Behavioral Health Challenges
Bridging the Gap between Physical and Behavioral Well-being through Systematic Approaches

THE VBP Blog
August 17, 2023 – In the ever-evolving landscape of healthcare, the relationship between physical health and behavioral health is gaining significant attention. Behavioral health encompasses both mental illnesses and substance use disorders (SUDs). It remains a focal point in achieving optimal health outcomes.
But how is managed care being used as a tool to address behavioral health? In this blog, the first of our Behavioral Health Series, we delve into the connection between physical and behavioral health, how managed care is making strides in this space, and what we expect to see in the future.
The Connection Between Physical and Behavioral Health
The goal of the healthcare system is to ensure that individuals can achieve their optimal health outcome, that is, they can be as healthy as possible. For too long, the focus has been on physical health with behavioral health becoming an afterthought. That is no longer the case.
The interdependence of physical and behavioral health is backed by compelling data. Studies have consistently shown that mental health, a large component of behavioral health, has been closely linked to overall health according to numerous studies, including one by Anne M. Doherty and Fiona Gaughran in Social Psychiatry and Psychiatric Epidemiology. Poor mental health can lead to poor physical health and this is true in many cases. One example is that depression has been linked to chronic illnesses, including diabetes, cancer, cardiovascular disease, and arthritis. Studies have also linked schizophrenia to a higher risk of respiratory and heart diseases. These are just a few examples of how behavioral health can impact physical health.
On the flip side, physical health also impacts behavioral health. Individuals that suffer from a heart attack or that are diagnosed with cancer often report feeling depressed or anxious. One report from the Cleveland Clinic discusses how thirty-three percent of people with a serious medical condition reported symptoms of depression, including sleep problems, loss of interest in daily activities, and poor mood.
As you can see, there is a strong link between physical and behavioral health. The consequences of unaddressed behavioral health concerns spill over into physical health and lead to poorer health outcomes. In addition to health outcomes, the National Alliance on Mental Health estimate that untreated mental health issues cost the United States up to $300 billion annually due to lost productivity. And, as many as 90 percent of suicide cases are attributed to mental health. Simply put, the convergence of physical and behavioral health isn’t merely a healthcare issue – it’s a societal concern that requires timely action.
State-led Initiatives – The Managed Care Approach to Behavioral Health
Now that we know how important it is to address behavioral health in connection with physical health, what is being done about it? The answer to that question is, it depends. States maintain flexibility in the coverage they offer, how the care is delivered, and how those services are paid out. However, many have been progressively turning to managed care to streamline and enhance the delivery of behavioral health services and they’ve been doing so using a variety of models.
This is an important issue for states because behavioral health conditions are particularly prevalent among Medicaid enrollees. In fact, studies show that around 39 percent of Medicaid enrollees live with such a disorder, and Medicaid is the single largest payer of behavioral health services in the country. And to exasperate things even further, Medicaid enrollees with behavioral health needs also have a higher prevalence of chronic conditions, which reduces their overall health and increases cost of care.
While some states still use a fee-for-service (FFS) model, many have turned to managed care with to address behavioral health with managed care organizations (MCOs) providing these services in recent years. That’s because integrating behavioral and physical health can enhance care coordination, improve health outcomes, and reduce costs for the high-need population. It’s important to note that many states, in fact, nearly all states in a recent Kaiser Family Foundation study from 2022, reported having multiple behavioral health delivery system models in place. The most common behavioral health deliver models in the country as of the study from 2022 are FFS and MCO.
Looking further into the KFF study, we also see that most states are relying on MCOs to administer and manage inpatient and outpatient behavioral health services. In the past states used to carve behavioral health services out of MCO contracts, but recent years have seen states carve these services into MCO contracts. The chart below from the KFF study shows the MCO coverage of behavioral health services based on different services.
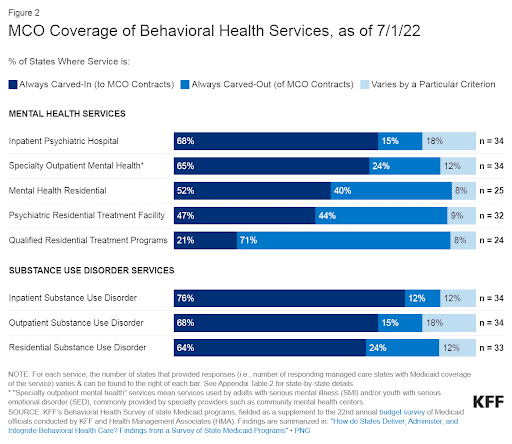
Source: KFF’s Behavioral Health Survey of state Medicaid programs
Even states that are utilizing Medicaid managed care to address behavioral health are doing so in different ways. The earliest adopters of managed care for behavioral health, Arizona, Florida, Kansas, New York, and Texas, used different approaches. Kansas and Texas carved in behavioral health services into managed care plans. While the states allowed managed care plans to subcontract with behavioral health organizations (BHOs) for behavioral health needs, they still bore the risk for managing the benefits. Arizona and Florida took a different approach, with integrated models designed specifically for individuals with SMI. In these states, specialty plans enrolled those with SMI or other serious BH needs to provide integrated care. New York stood alone using a hybrid approach where the state carved in all behavioral health services in their managed care plans.
More recent states to adopt Medicaid managed care for behavioral health also use different approaches. California is using its CalAIM Section 1115 waiver initiative to improve coordination of mental health care between MCOs managing non-specialty mental health services and county-operated mental health PHPs managing specialty mental health services and SUD treatment. Ohio is taking a different approach by implementing a specialized managed care entity that is responsible for providing behavioral health services to those enrolled in both MCOs and FFS. While states vary in their approach, most allow MCOs to use their “in lieu of” authority to cover certain behavioral health services.
As you can see, there is no one-size fits all model for implementing managed care to address behavioral health. What matters is that care coordination is stressed and that the emphasis is placed on improving overall health outcomes.
Advocates Perspective
While progress is being made, despite state and federal efforts to improve accessibility and quality, approximately 35 percent of Medicaid beneficiaries with significant mental health concerns report not receiving treatment. There are many reasons for this, but the number is still too high. Behavioral health, with its proven link to physical well-being, societal functioning, and overall health, demands more attention. Managed care is emerging as a promising solution, but as states continue to innovate and refine their strategies, we need to continue progressing to ensure that everyone has access to care. IN addition, it is essential that behavioral and physical health are not being treated in siloes, rather care is being integrated so all needs of an individual are met.
Onward!
The Behavioral Health Series – What’s Next?
As the behavioral health arena continues to evolve, our Behavioral Health Series is the place to look for updates and industry trends. We will address topics like the challenges to utilizing managed care for behavioral health, how companies that work in multiple states and can utilize knowledge and platforms from one state to another, how ACOs are integrating behavioral health, how states are expanding access to behavioral health services, and more! Keep an eye on the VBP blog for more insights and information!
Share This Blog!
Get even more insights on Linkedin & Twitter

About the Author
Fady Sahhar brings over 30 years of senior management experience working with major multinational companies including Sara Lee, Mobil Oil, Tenneco Packaging, Pactiv, Progressive Insurance, Transitions Optical, PPG Industries and Essilor (France).
His corporate responsibilities included new product development, strategic planning, marketing management, and global sales. He has developed a number of global communications networks, launched products in over 45 countries, and managed a number of branded patented products.

About the Co-Author
Mandy Sahhar provides experience in digital marketing, event management, and business development. Her background has allowed her to get in on the ground floor of marketing efforts including website design, content marketing, and trade show planning. Through her modern approach, she focuses on bringing businesses into the new digital age of marketing through unique approaches and focused content creation. With a passion for communications, she can bring a fresh perspective to an ever-changing industry. Mandy has an MBA with a marketing concentration from Canisius College.