A New Era of Medicaid Managed Care Transforming IDD Care in Florida
Florida’s innovative Medicaid Managed Care pilot program aims to reshape healthcare for individuals with Intellectual and Developmental Disabilities (IDD)
THE VBP Blog

March 15, 2024 – Florida is set to launch its Managed Care pilot specifically designed for individuals with Intellectual and Developmental Disabilities (IDD) this year. This innovative program offers a more coordinated, comprehensive approach to meet the diverse needs of this population. The pilot is a significant milestone for Florida, reflecting a commitment to ensuring that individuals with IDD receive the support and services they require in a manner that respects their individuality and promotes their well-being.
This blog will explore the specifics of the pilot program, its objectives, and the anticipated benefits for enrollees. As advocates, we are excited to see the advancement of value-based payments in the IDD sphere and that the selected managed care organization (MCO) is provider owned but know that careful consideration needs to be placed on stakeholder involvement in implementation to ensure a smooth shift for both consumers and providers. It is also concerning that the pilot is being conducted with one MCO, which can limit consumer choice and learning from the pilot. To learn more about our advocate’s perspective, check out our full write up at the end of the blog to learn more on our thoughts of how this initiative will impact consumers and quality of care!
Florida’s Medicaid Managed Care Designed to Provide Person-Centered Care
In November of 2023, the Florida Agency for Healthcare Administration (AHCA) released an invitation to negotiate (ITN) for the Comprehensive Intellectual and Developmental Disabilities Managed Care Pilot Program (Pilot Program). The pilot program takes place across two regions and is designed to provide a more coordinated, comprehensive, and person-centered care model. The pilot is set to launch in 2024 and run for six years through September 30, 2030.
Both Simply Healthcare Plans, Inc. and Florida Community Care submitted responses to the ITN. It was announced that Florida AHCA intends to award the six year contract to Florida Community Care, who already holds contracts to provide Medicaid Long-Term Care Plus plans in the state.
Through the IDD managed care pilot, 600 beneficiaries will receive comprehensive medical, long-term care (LTC) and home- and community-based services (HCBS) waiver services under a managed care model. In Florida, people with IDD currently receive these services on a fee-for-service (FFS) basis through the Developmental Disabilities Individual Budgeting (iBudget) waiver. This means that services are provided and billed based on the quantity provided, not the quality. For some, this can mean getting duplicate or unnecessary services as providers are compensated based on the number of services they provide. There is also no incentive for providers to coordinate care as they all operate in their own silos due to reimbursement.
Under the new pilot program, selected providers will provide comprehensive IDD services to eligible individuals through a managed care delivery system. This will ultimately become a value-based payment model that rewards providers based on the quality of care beneficiaries receive, as well as their health outcomes. The program’s objective is to provide comprehensive medical, long-term care for individuals with IDD. According to the ITN, the specific goals of the pilot include:
- Maximizing managed care flexibility to provide additional services
- Increase access to providers and services
- Maintain highest quality of care coordination and person-centered care plans
- Increasing opportunities for community integration
There are several ways the pilot aims to reach these goals. The first is through an emphasis on person-centered planning. This approach tailors care plans to the individual’s specific needs, preferences, and goals, recognizing that each person with IDD has unique circumstances. The Managed care organization (MCO) will be tasked with developing and implementing these personalized care plans, working closely with consumers / members, families, and a network of providers to ensure comprehensive support across all areas of life.
Not only is there a list of services that an MCO must provide, but there is also something called “expanded benefits” in the ITN that are benefits covered by the Managed Care Plan for which the Managed Care Plan receives no direct payment from the Agency. These benefits can boost health outcomes, improve independence enhance social inclusion, and boost quality of life, and include things like:
- Therapies unique to the IDD population, such as music therapy, art therapy, swim safety and therapy for adults and children
- Specialized camps
- Services to support caregivers
- Transition planning services to assist as caregivers age
- Gym memberships
Another significant aspect of the pilot is the enhanced access to providers and services. Respondents to the ITN needed to provide staff and enrollee ratios for care coordinators and other administrative positions like provider relations and claims resolution. They also needed to provide a list of providers that met certain capacity requirements to show they had the capability of meeting the needs of the 600 beneficiaries selected for the pilot.
Potential Benefits and Challenges for IDD Medicaid Beneficiaries
There are many benefits to moving individuals with IDD under a managed care program. One of the primary advantages of managed care is its emphasis on coordinated, comprehensive healthcare services. Individuals with IDD often require a wide range of medical, behavioral, and support services. Managed care can facilitate better communication among providers, resulting in more cohesive care plans and potentially better health outcomes. Another benefit is the pilot’s focus on tailoring care plans to the individual’s needs, preferences, and goals. This approach can improve satisfaction and engagement among beneficiaries, ensuring that services are more aligned with their desired outcomes.
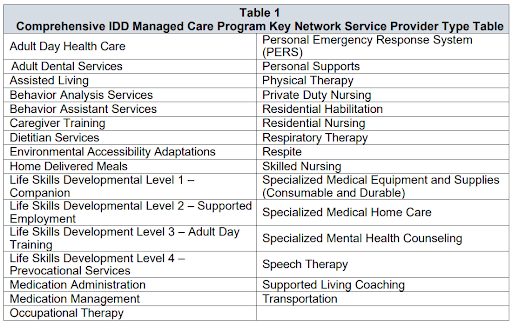
As you can see from Table 1 of the ITN below, there is a wide range of services that the provider network will need to encompass.
The pilot program also has a focus on improving access to services. Many individuals requiring these services are placed on wait lists, which limits their ability to live independently at home and remain an active member of the community. Through the pilot program, the managed care organizations (MCOs) are incentivized to create networks of providers that can meet the diverse needs of their enrollees. In fact, of the possible 1,000 points awarded through the ITN process, increasing access to providers and services made up for 20% of the total score. Community partnership was another 10% of the score, which also helps increase access to services, meaning that expanding access to services makes up approximately one third of the total score. That shows how important improved access to specialty services, therapies, and community-based support are because they are all crucial for the well-being of individuals with IDD.
While there are many benefits to a managed care program for individuals with IDD, there are some challenges that need to be highlighted. The first is that managed care involves budget caps and fixed payments. If not implemented properly, this can lead some MCOs to limit access to certain services to control costs. This poses a risk that beneficiaries might not receive all the services they need, or that access to high cost but necessary treatments could be restricted. To mitigate this, quality measures that incentivize providers to offer these services need to be considered. One way the pilot program aims to combat this is through the Quality Withhold Incentive. Each year, 2 percent of the MCO’s capitation rate will be withheld and can be earned based on the MCO’s performance according to specific performance measures compared against national performance standards.
Another aspect to consider is the continuity of care. The success of managed care hinges on the quality of the provider network and the continuity of care. There’s a risk that changes in Medicaid management could disrupt existing patient-provider relationships or lead to variations in the quality of care provided by the MCO. There is also concern that the network selected by the single MCO in this pilot will limit consumer choice as they have no say in the network selected. This also means that is the quality of care they receive from the MCO network is not adequate, there are no alternative providers they can turn to. The iBudget waiver also gives consumers much control over where they spend their allocated budget. While consumers don’t get to pick and choose where they spend their budget under the new managed care contract, there are care coordinators in place to ensure that consumers get the services they need.
In addition, the transition to a managed care model can introduce administrative challenges for providers and beneficiaries. Navigating new processes for service authorization, appeals, and grievances can be challenging so there needs to be proper education and outreach to both providers and beneficiaries to ensure access to care is not limited.
While the Managed Care pilot program for Medicaid beneficiaries with IDD in Florida has the potential to significantly improve the coordination, access, and personalization of care, it also introduces challenges that need to be carefully addressed. Success will depend on the state’s ability to ensure that MCOs prioritize the needs of beneficiaries over cost-saving measures, maintain high-quality provider networks, and manage the transition in a way that minimizes disruptions to care.
Advocates Perspective
Florida is not alone in its shift to managed care for the IDD population. Many other states have launched the own IDD managed care programs, each with varying degrees of success. What is clear from these programs is that there is not a one-size-fits-all approach. While states are beginning to take notice and realize that value-based payments can have a significant impact on quality of care, especially for individuals with complex needs, each state is putting its own unique twist on their models. While Florida’s pilot program underscores a commitment to enhancing the quality of life for this vulnerable population through a coordinated, comprehensive care model, we are concerned that there is only a single MCO conducting the pilot program. This can limit consumer choice and may also limit the learning that is possible from this pilot. However, on a positive note, FCC is provider owner, which will put providers at the front line of monitoring and ensuring that consumers are getting the quality care they deserve. As the state moves forward with implementation, the focus is now on transparency, accountability, and quality outcomes.
Onward!
Share This Blog!
Get even more insights on Linkedin & Twitter

About the Author
Fady Sahhar brings over 30 years of senior management experience working with major multinational companies including Sara Lee, Mobil Oil, Tenneco Packaging, Pactiv, Progressive Insurance, Transitions Optical, PPG Industries and Essilor (France).
His corporate responsibilities included new product development, strategic planning, marketing management, and global sales. He has developed a number of global communications networks, launched products in over 45 countries, and managed a number of branded patented products.

About the Co-Author
Mandy Sahhar provides experience in digital marketing, event management, and business development. Her background has allowed her to get in on the ground floor of marketing efforts including website design, content marketing, and trade show planning. Through her modern approach, she focuses on bringing businesses into the new digital age of marketing through unique approaches and focused content creation. With a passion for communications, she can bring a fresh perspective to an ever-changing industry. Mandy has an MBA with a marketing concentration from Canisius College.
